April 22, 2024
Substance use disorders are underdiagnosed and undertreated among formerly incarcerated Virginians, new VCU-led study finds
Research collaboration with the Virginia Department of Medical Assistance Services highlights health disparities affecting Medicaid members with addiction – and some of the barriers they face.
Share this story
People recently released from prison experience some of the highest rates of substance use disorder, but they are also the least likely to have access to providers who can diagnose and treat their addiction. New research led by Virginia Commonwealth University’s School of Population Health is shedding light on the magnitude of these health disparities in Virginia and what policies might help people receive lifesaving care.
National estimates suggest as many as 85% of people who are incarcerated have substance use disorders. While most of these adults are eligible for Medicaid services after their release, the VCU-led study found that only 17% of formerly incarcerated Medicaid members were diagnosed with substance use disorders in Virginia. Even fewer received medications as treatment for their addiction.
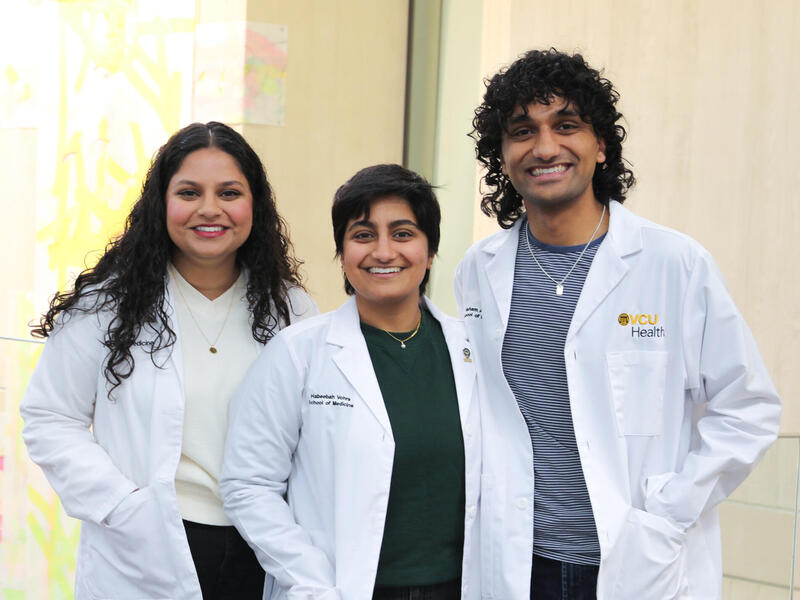
“We know that substance use disorders are prevalent health issues among incarcerated populations, but this research shows that many people aren’t getting the medical attention they need as they transition back to their communities,” said Peter Cunningham, Ph.D., who led the new research and is interim chair of the Department of Health Policy at VCU’s School of Population Health. Other contributors to the report include Sarah Marks and Hannah Shadowen – both M.D.-Ph.D. students at VCU’s School of Population Health – as well as Peyton Bernstein, a master’s student at the College of William & Mary.
The study is part of a collaboration between VCU and the Virginia Department of Medical Assistance Services to better understand health disparities impacting Medicaid members with opioid and other substance use disorders. Using data from both DMAS and the Virginia Department of Corrections, the researchers measured the number of people being diagnosed and treated for a substance use disorder following their release from prison.
According to the VCU research team’s analysis, 4,652 adults were released from county jails and state prisons in 2022, with 85% enrolling in Medicaid within one month of release. Among those enrolled in Medicaid, only 17% had seen health care providers and were diagnosed with a substance use disorder within three months, including 13% with an opioid use disorder.
Of those who were formerly incarcerated and diagnosed with an opioid use disorder, only about 25% went on to receive medications to treat their addiction. By comparison, 78% of all Medicaid members diagnosed with an opioid use disorder in Virginia received medications.
“The good news is that we see a high number of individuals enrolling in Medicaid soon after they are released from prison, and that is in large part due to the state expanding Medicaid coverage in 2019,” Cunningham said. “However, based on national statistics, we expected more people to receive a diagnosis and treatment for opioid addiction. This is concerning because having an undiagnosed, untreated opioid use disorder greatly increases the risk of overdose.”
The researchers noted that a number of barriers might be contributing to these gaps in addiction treatment, such as the instability many formerly incarcerated adults experience after their release, as well as limitations in access to Medicaid services set by federal policies.
While the vast majority of individuals in the criminal justice system qualify for Medicaid, only emergency hospital services are covered as they serve their sentence. Most other benefits – including treatments for substance use disorders – are prohibited by federal law until after a person is released from prison.
“The first few months after a person is released from incarceration is a particularly vulnerable time. They often have to figure out all aspects of their life at the same time,” said Shadowen. “Many people don’t have a stable residence, mailing address or phone number, which makes it difficult for the Medicaid agency to contact them for health services.”
“It can also take some time for a person to be registered as eligible for Medicaid and schedule an appointment with a provider,” added Marks. “Even having the required photo identification and Medicaid card to visit a doctor’s office is going to be much harder to do during this period of tremendous instability.”
Increasing access to treatment prior to release can help to facilitate transitions to the community and ensure continuity of treatment following release from incarceration, Cunningham explained. “If providers are able to diagnose substance use disorders and initiate treatment plans before a person is released from prison, this might reduce the risk of overdoses and improve health outcomes when they return to their community.”
Looking ahead, the researchers are surveying formerly incarcerated Medicaid members to pinpoint some of the barriers they experience when seeking addiction treatment after prison.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.