May 25, 2017
Researchers across the state to participate in Virginia Drug Consortium’s VirginiaCancerRx Symposium
The two-day event could spark collaborations on cancer drug discoveries.
Share this story
The Virginia Drug Discovery Consortium’s VirginiaCancerRx symposium will bring together Virginia’s most innovative cancer researchers, with the aim of devoting expertise to developing cancer fighting drugs and insights into disease pathways.
The VaDDC, of which Virginia Commonwealth University is a participant, will host the event, which will include presentations from more than two-dozen researchers at VCU, the University of Virginia, Virginia Tech and other research institutions across the commonwealth. Nationally recognized keynote speakers from the American Cancer Society; Janssen Research & Development, LLC; and The Johns Hopkins University School of Medicine will also participate in the symposium, held at the University of Virginia Darden School of Business from May 30–31.
“We aim to facilitate collaborative drug discovery, development and delivery in the commonwealth, and to translate drug research into important medicines or devices,” said co-organizer Nicholas Farrell, Ph.D., a professor in the Department of Chemistry in the College of Humanities and Sciences and a member of the Developmental Therapeutics research program at VCU Massey Cancer Center. “The consortium aims to emphasize the benefits of building on the mutual strengths and common interests of Virginia’s universities.”
The event could also strengthen Virginia’s pharmaceutical industry, said David Kingston, Ph.D, a distinguished professor in the Department of Chemistry at Virginia Tech and Virginia CancerRx symposium chair.
“Collaborative research on drug discovery between Virginia’s universities and research institutes will enhance drug discovery research and could become a significant economic force throughout the commonwealth,” Kingston said.
VirginiaCancerRx follows the successful VirginiaBrainRx symposium held in Richmond last year, which brought together pharmaceutical companies and researchers to develop therapeutics for the treatment of brain disease. The event fostered ongoing studies between faculty from VCU and other institutions.
“It’s a matter of seeking out who is doing what and where and trying to build on shared knowledge, and sometimes the connections are not that obvious,” said co-organizer Richard Glennon, chairman of the Department of Medicinal Chemistry in the School of Pharmacy.
VCU sponsors for Virginia CancerRx include the Office of Research and Innovation, the School of Medicine, Massey Cancer Center and the School of Pharmacy Office of Continuing Education. Other funders include the University of Virginia, George Mason University, INOVA Fairfax, Virginia Tech, Eastern Virginia Medical School, Promega Corporation, Advion and Thermo Fisher Scientific.
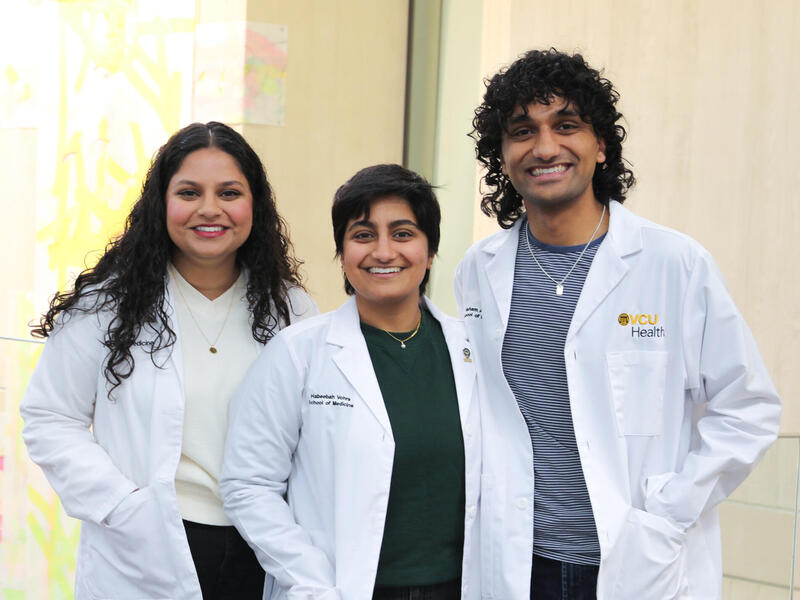
Five VCU researchers will present breakthroughs and developments in cancer therapeutics at the symposium:
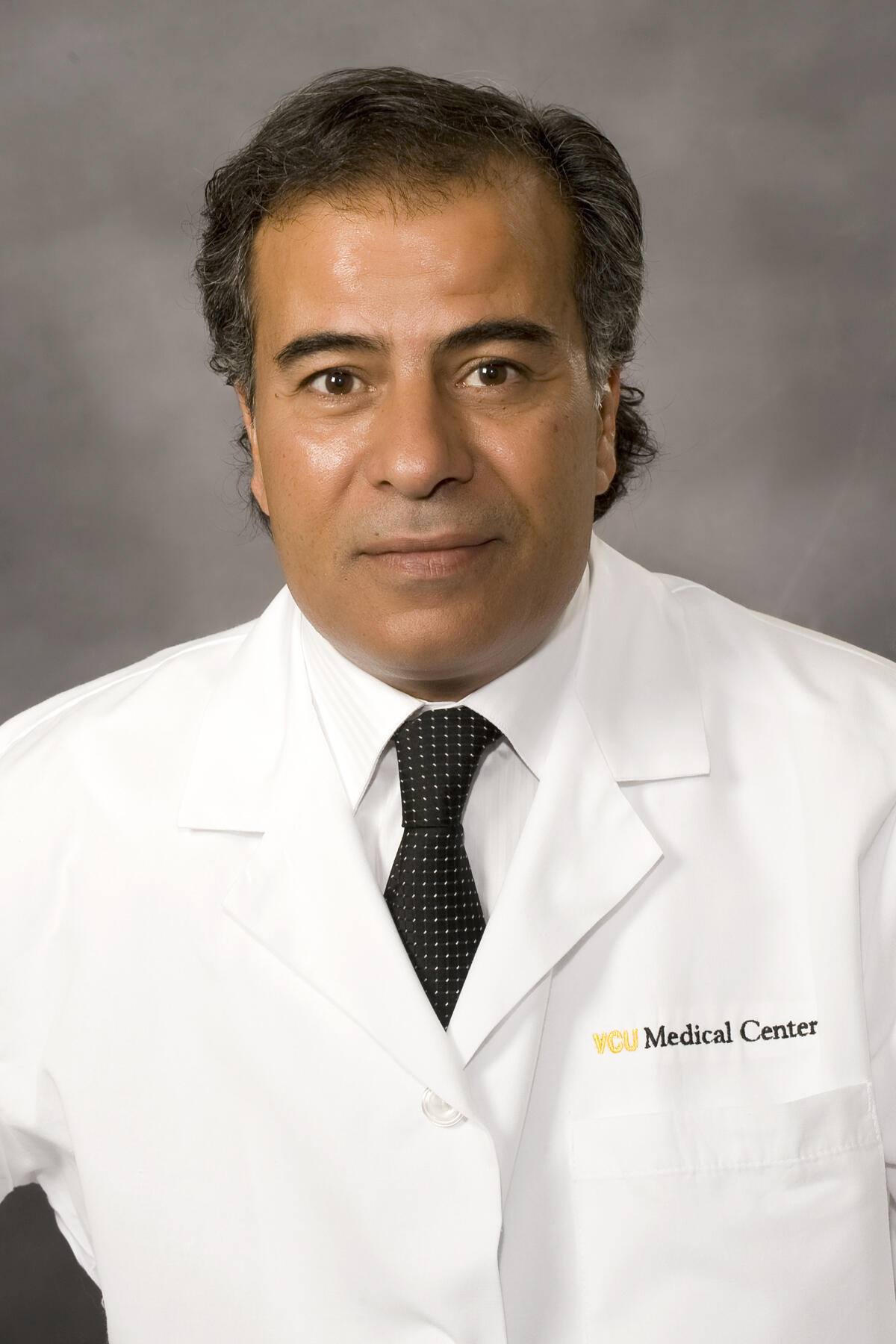
Jamal Zweit, Ph.D., professor in the Department of Radiology at the VCU School of Medicine, director of the Center for Molecular Imaging and a member of the Developmental Therapeutics Program at Massey Cancer Center.
Zweit is developing a drug derivative that can fight cancer and be observed in real time as it works in the body. Zweit’s lab has crafted fluorine-18-carboplatin, a modified platinum-based drug. About half of all cancer patients who undergo chemotherapy receive platinum-based drugs. What is unique about Zweit’s drug is it contains an additive that could enable it to be viewed in vivo via a molecular imaging technique. Physicians would be able to directly observe how effectively the drug is targeting tumors.
The aim is to assess what quantity of an intravenously delivered chemotherapy travels to a specific tumor site, and how much of the drug remains at the site, Zweit said. This new tool could also guide genetic and protein analysis of tumors in order to assess why drugs are more likely to accumulate and be retained in some regions of tumors compared to others.
“Just imagine the power of this,” Zweit said. “You are looking at a complete picture of the drug in a live patient and observing its accumulation with time. It is a direct way to noninvasively determine how the drug is doing on an individual patient basis, and who is likely to respond to such therapy.”
Observing platinum-based drugs in vivo would assist physicians in tailoring specific treatments to individual patients. Tumor characteristics vary between patients, and even within the body of a single person in regard to chemotherapy response.
Further development of fluorine-18-carbonplatin is ongoing in collaboration with the Women’s Health Research Institute at Inova Fairfax.

Nicholas Farrell, Ph.D., professor in the Department of Chemistry in the College of Humanities and Sciences and member of the Developmental Therapeutics research program at VCU Massey Cancer Center.
Farrell has found that a new class of platinum-based drugs may be particularly effective against metastatic cancer. Polynuclear platinum-based drugs are able to identify new targets in tumor cells, which were previously non-receptive to platinum-based anticancer drugs. Farrell’s findings mean that more types of cancer may be treatable by these drugs, and could also lead to the development of more cancer fighting drugs.
“We think our findings are very significant because it gives a whole new direction to platinum-based drugs,” Farrell said. “And it gives us a whole new understanding of what was going on with the original drugs. It’s an area that might have been overlooked for 30 years. It’s opening up a whole new avenue of research for platinum-based drugs.”

Steven Grossman, M.D., Ph.D., chair of the Division of Hematology, Oncology and Palliative Care in the Department of Internal Medicine at the School of Medicine and deputy director at Massey Cancer Center.
Grossman has discovered that a protein that contributes to the growth of cancer cells may be an effective target for the development of cancer-fighting drugs.
Grossman’s findings are centered on C-terminal binding protein, or CtBP. The protein is well-known for its role in regulating gene expression in cancer cells. Gene expression is a cellular process that controls how many proteins are made and when, which is a key factor in cancer metastasis and growth. CtBP is also produced in almost all types of common solid human malignant tumors.
The protein may be a particularly successful drug target because of its unique ability to bind to small molecules. Grossman is developing CtBP inhibitors tailored to this characteristic, which would consist of synthetic small molecules harmful to the protein.
“In a way, the binding characteristic is the Achilles’ heel of this protein. The synthetic small molecules would look like natural ones, but are a Trojan horse,” he said. “We are tricking it by giving it something that looks like what it wants but it’s poison to this particular protein while otherwise not affecting other normal proteins in the cell.”
CtBP may also hold the key to targeting cancer stem cells, which are in low abundance in tumors but may fuel the ability of many tumors to resist chemotherapy. Cancer stem cells could possibly be dormant after curative surgeries and spark postsurgical relapse and metastasis.
Grossman’s lab has developed a third generation of inhibitors, which have been shown to deter the formation of tumors in mice.
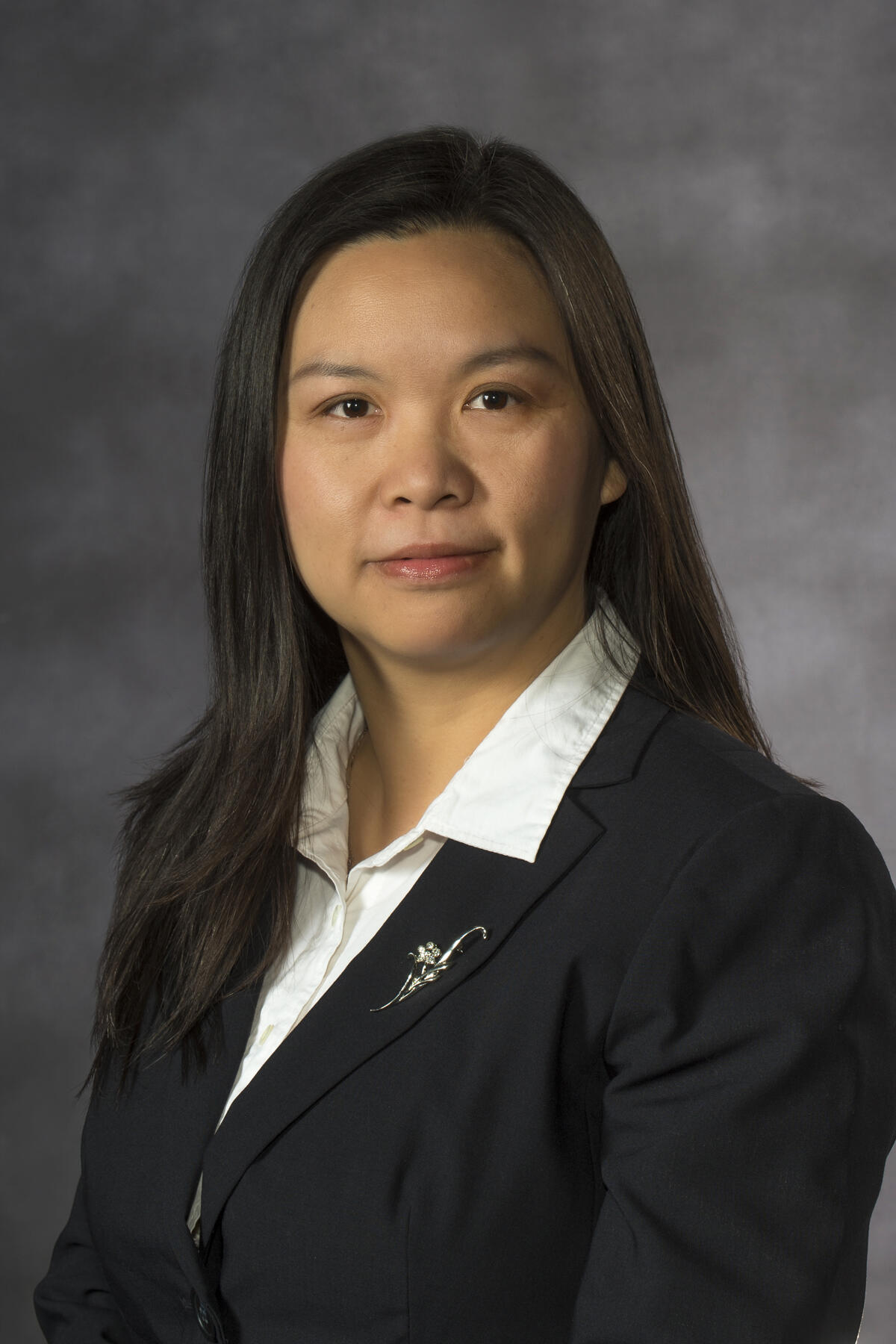
Rong Huang, Ph.D., assistant professor in the Department of Medicinal Chemistry in the School of Pharmacy and member of Developmental Therapeutics research program at Massey Cancer Center.
Huang is unlocking clues about the biochemical pathways of protein N-terminal methyltransferases, or NTMTs. Discovering how the protein interacts with other enzymes to bring about biochemical reactions may lead to identification of new targets and the development of anticancer drugs, Huang said.
Little is known about the network of NTMT, which is found to have a role in functions such as cell division and DNA repair. The protein has a high rate of expression in the tumor tissue of patients.
Huang and her lab are working to develop NTMT inhibitors, which halt the activity of NTMT. The purpose would be to obtain a greater insight into the downstream effects of NTMT.
“We are developing an inhibitor that would help us gain basic knowledge and maybe try to elucidate all of the networks in which NTMT is involved,” Huang said. “Hopefully once we understand the basic knowledge we can use this inhibitor to eventually develop an anticancer drug. Everything is still at an early stage.”
Umesh Desai, professor in the Department of Medicinal Chemistry in the School of Pharmacy and member of Developmental Therapeutics research program at Massey Cancer Center.
Desai is researching whether G2.2 — a molecule engineered by his lab — could stop the spread of cancer and kill existing cancer cells.
Tests in small animal models show G2.2 kills cancer stem cells. Desai and his collaborator Bhaumik Patel, M.D., an associate professor in the Division of Hematology, Oncology and Palliative Care at the School of Medicine and a member of the Developmental Therapeutics research program at VCU Massey Cancer Center, have found that G2.2 may affect cancer stem cells because it changes the function of certain types of glycosaminoglycans, or GAGs, which are types of biopolymers present on all cell surfaces. Biopolymers are large molecular structures found in living organisms and are composed of similar units.
Desai said these GAGs typically contribute to the proliferation of cancer cells and G2.2 may inhibit GAG influence.
“Basically, what the cancer stem cells do is keep dividing and that is how they generate new cells. Think about a lawn and how sprinklers provide nourishment for the lawn. If you have these sprinklers turned on, you are going to have a lush, green lawn,” Desai said. “If you turn off the sprinklers — the type of GAGs in this case — there is basically no more cell division."
Desai and Patel theorize these GAGs are recognized by certain protein receptors on cancer stem cells, which contribute to growth and metastasis. G2.2 would work by turning off or changing the function of these receptors. The cancer stem cells would die and not replicate.
Targeting cancer stem cells over other types of cancer cells — called bulk cells — may hold the key to preventing relapse, Desai said.
Subscribe for free to the VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Monday and Thursday.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.