May 31, 2024
Drug candidate shows promise in easing chronic pain, new study finds
Share this story
A team of researchers from Virginia Commonwealth University, the University of Texas at Austin and the University of Virginia have made progress toward developing a drug candidate for treating chronic pain more safely.
Chronic pain afflicts millions of people, but for many, a reliable, nonaddictive drug to ease their suffering remains out of reach. Some of the most effective drugs for treating severe pain, opioids, are highly addictive and have led to public health crises of substance use disorder and overdoses.
In their most recent study, published in Proceedings of the National Academy of Sciences, the researchers found that the drug candidate was able to effectively trick immune systems in such a way as to shut off an inflammatory response, thereby alleviating pain. While this research is currently at the preclinical stage, the ultimate goal is to make an effective and targeted treatment for people suffering from chronic pain.
Promising drug candidate sparks collaboration
Immune cells in the human body produce compounds called endocannabinoids that, among other things, regulate inflammation. In a healthy person, inflammation is a process that helps the body heal from infections or injuries. But the downside is that it also causes swelling and buildup of tissue that presses on nerve endings and causes persistent pain.
“When the endocannabinoids in our bodies cause inflammation, our nerves become sensitized. They react more rapidly with less stimulation than what is normally needed. This causes things that normally wouldn’t hurt to suddenly become extremely painful, similar to how we feel when we have a bad sunburn,” said Aron Lichtman, Ph.D., a professor in VCU School of Medicine’s Department of Pharmacology and Toxicology.
In this study, the researchers analyzed an inhibitor called KT109 that blocks the activity of a endocannabinoid-producing enzyme in immune cells called DAGLβ.
Ken Hsu, Ph.D., an associate professor in the Department of Chemistry at UT Austin, developed the inhibitor in 2012 as a postdoctoral fellow at The Scripps Research Institute. He has since fostered a long-term collaboration with Lichtman and Hamid Akbarali, Ph.D., also a professor in VCU’s Department of Pharmacology and Toxicology, to better understand how inhibiting DAGLβ reduces inflammation and the associated pain.
Akbarali’s expertise is investigating how inflammation impacts the nervous system at the cellular level. His research team examined how the drug candidate interfered with pain-transmitting neurons in mouse models.
“In our lab, we look at the speed and strength of the pain signals that neurons send to the brain, and for this particular project, we analyzed how the drug candidate weakened these signals as they traveled through the nervous system,” he said.
Lichtman’s research team focused on understanding how these cellular processes then impact the behavior and function of mice with chronic pain.
“Our process has really been a bottom-up discovery. This research originally started with understanding the inhibitor at the molecular level, while this new study aimed to better understand how the inhibitor has an impact at the cellular and behavioral level,” Lichtman said.
Uncovering the pathway to pain relief
Previous work demonstrated how KT109 controls inflammation via endocannabinoids and prostaglandins. But in this latest study, the researchers were surprised to discover that it also controls inflammation through an additional pathway, which helps explain why the inhibitor is effective in treating different types of pain.
“When you inhibit DAGLβ, your immune cells are tricked into thinking they are starving,” Hsu said. “Changes in energy metabolism in the immune system can turn off inflammatory signaling and be effective in pain management. One example is the drug metformin,” which is commonly used to treat diabetes but also has been found effective in treating pain.
The team’s inhibitor targets the enzyme DAGLβ, which is mainly present and active in immune cells, thereby avoiding any unnecessary reaction with other cells that might lead to side effects.
“You’re going to affect these pathways where it matters, where the inflammation is happening,” Hsu said.
The researchers don’t believe this drug inhibitor acts in the brain, thereby avoiding the potential alteration of reward pathways in the brain that might lead to substance abuse.
The research team has so far only studied the effects of the inhibitor through injection, but the goal is to develop a pill that can be swallowed, as a human would ingest a drug compound. To avoid internal toxicity, the researchers will aim to refine the chemistry and reduce the number of times the medicine needs to be taken while maintaining the same pain-easing effect.
The findings are helpful for pharmaceutical companies considering the development of medicines that target DAGLβ in people experiencing chronic pain.
A shared mission in ending addiction
Akbarali and Lichtman noted that their teams’ contributions to this discovery were made possible through the strength of VCU’s infrastructure for addiction research.
The project received significant support from the Central Virginia Center on Drug Abuse Research, an interdisciplinary research center based at VCU that is focused on addiction to opioids and other drugs of abuse. Fueled by a $6.8 million grant from the National Institute on Drug Abuse, the center provides funds and resources to advance promising research aimed at addressing addiction.
The two investigators also credited the wealth of resources at VCU for training the next generation of scientists to tackle drug abuse.
Many of the graduate students and postdoctoral researchers who contributed to this study are funded through a T32 grant from NIDA. VCU’s Department of Pharmacology and Toxicology initially secured the federal grant in 1976 to provide tuition, equipment and supplies to those training to be addiction researchers. The grant has been renewed every five years ever since, providing roughly $24 million in support to more than 600 students and trainees over the past five decades.
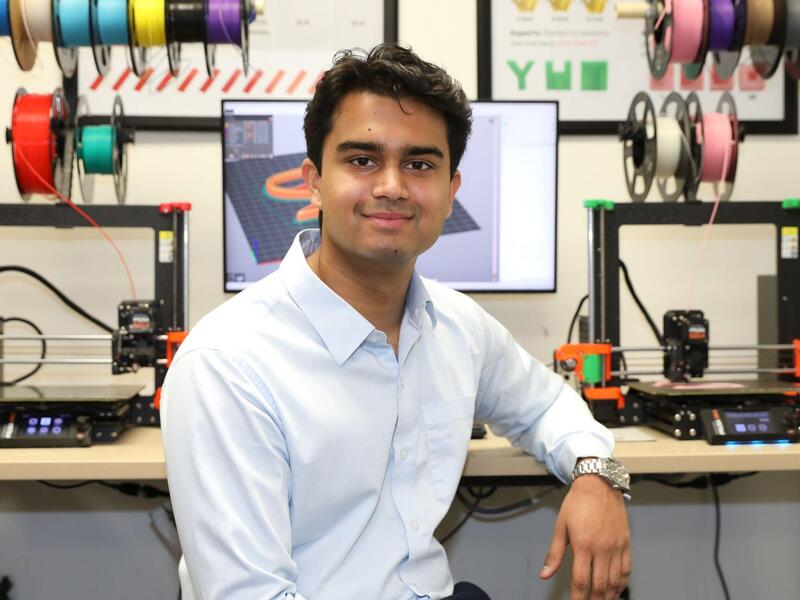
One of the students involved in this study is Mohammed Mustafa. He manages the logistics and operations for Lichtman’s research lab while also working toward his Ph.D. in pharmacology and toxicology.
Mustafa first became interested in the endocannabinoid system when he was an undergraduate student at VCU. Now he studies this system to help identify treatments for chemotherapy-related pain. Because of his expertise, he was enlisted to help coordinate data collection for the study, along with Giulia Donvito, Karan Muchhala and Ryan Mischel.
“Being brought in to this study has been very beneficial for my own research projects, as it’s exposing me to new perspectives and skills that I’ll end up applying as I work toward my doctoral degree. Projects like these keep you competitive and have helped grow my confidence as an early career researcher,” Mustafa said. “It was also great to be a part of a research effort that involved multiple labs from different institutions. You have to have these kinds of collaborations to make science happen.”
At VCU, students and trainees are given opportunities to join cutting-edge projects that build their knowledge on addiction research and other subjects.
“By being involved in our study, not only are they learning important skills in biomedical research, but they also get to be an author on a high-impact journal, which will help them move forward in whatever career they decide to take in the future,” Akbarali said.
“Our studies also benefit from student involvement because they are the conduits of research and collaboration,” Lichtman added. “They are the ones actually at the bench doing this important work.”
This article is a modified version of a release from UT Austin. The original version can be found here.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.