July 1, 2016
Drug that targets multiple drug-resistant strains of HIV and other viruses is ready for clinical trials
Share this story
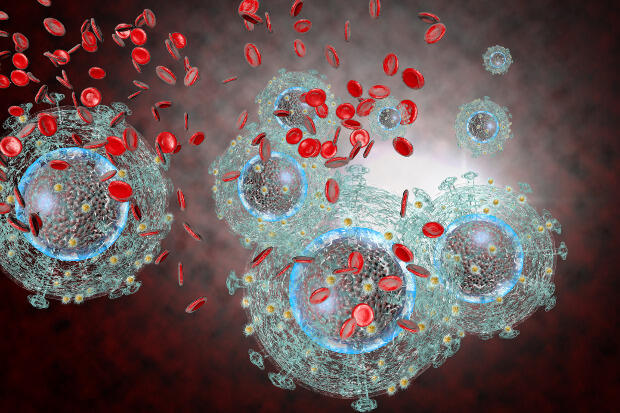
A research team spanning four continents has detailed the anti-viral capabilities of OSU-03012, also known as AR-12, a drug currently used in clinical trials to treat certain cancer tumors. The present study confirms that AR-12 is effective in treating a host of viral infections in the laboratory and in animal models, including multiple strains of drug-resistant HIV, Ebola, influenza, mumps and measles.
The paper was published last month in the Journal of Cell Physiology, and authors contend that new clinical trials as an anti-viral drug are warranted.
Basically, we have fully worked out how the drug works and why it stops so many different kinds of virus.
“Basically, we have fully worked out how the drug works and why it stops so many different kinds of virus,” said lead researcher Paul Dent, Ph.D., professor in theDepartment of Biochemistry and Molecular Biology at Virginia Commonwealth University School of Medicine and Universal Chair for Signal Transduction.
The research expands on a paper published last year showing the efficacy of AR-12 combined with phosphodiesterase type 5 inhibitors like Viagra and Cialis at targeting GRP78, which is a specific chaperone protein. The job of a chaperone protein is to keep enzymes and virus coat proteins in their correct three-dimensional shape. If an enzyme or coat protein has an incorrect 3-D shape, the enzyme does not work and the coat protein cannot form into a new virus.
Many researchers over the past 25 years have shown that GRP78 is essential for the replication of almost every type of pathogenic virus. The new study validates and extends the earlier findings.
In order for a virus to successfully replicate and take over a cell, two things have to happen: the virus has to be able to create a protective protein coating for production of “baby” viruses and it also has to hijack cell signaling so that the cell doesn’t know that it’s being stressed. When the cell is stressed, it can lead to process called autophagy, which is the cell killing itself, before new baby viruses have formed.
Researchers noted that AR-12, when used in combination with certain drugs, gets in the way of both of these processes by inhibiting chaperone proteins like GRP78. When chaperones are inhibited, the cell sends out a distress signal and autophagy begins. The cell begins to process the damaged virus coat proteins that have the wrong 3D shape — essentially eating up the virus coat protein. This prevents the virus from taking over.
In the new study, researchers noted that a wide range of chaperones are targeted with AR-12, not just GRP78.
“The real take home is there are two broad families of chaperones,” said Dent. “One is the HSP90 family and the other is the HSP70 family, and it turned out the AR-12 drug was able to stop the functions of both families.”
For some viruses, such as Junín, the Argentinian hemorrhagic fever virus, HSP90 and HSP70 were more important for the production of baby virus than the chaperone GRP78.
In animal models, AR12 doubled survival and suppressed liver damage caused by another hemorrhagic fever virus, effectively protected cells from Ebola and suppressed drug-resistant strains of HIV significantly more effectively than any of the approved anti-viral treatments.
Previously, researchers also confirmed AR-12’s efficacy in suppressing the reproductive capabilities of rabies, chikungunya, rubella, respiratory syncytial virus, Marburg, Lassa, Coxsackie, adenovirus, dengue, West Nile, yellow fever and enterovirus 71.
One of the most compelling observations was AR-12 suppressed the reproduction of multiple drug-resistant strains of HIV1 and HIV2. Dent speculates that adding AR-12 to an HIV patient’s current protease inhibitor cocktail would not only be more effective at controlling the disease but also that in the very long term patients might potentially be able to reduce their dosage of protease inhibitors, which tend to have more side effects than AR-12.
Dent collaborated on this study with Heath Ecroyd, Illawarra Health and Medical Research Institute in Australia; St. Patrick Reid, U.S. Army Medical Research Institute of Infectious Disease; Alexander Zukiwski and Stefan Proniuk, Arno Therapeutics; Abraham Jacob, University of Arizona Ear Institute; Claudia S. Sepulveda, Ciudad Universitaria in Buenos Aires; and Maria Tunon, at The University of Leon in Spain.
The full article is available online at http://onlinelibrary.wiley.com/doi/10.1002/jcp.25431/abstract.
Subscribe for free to the weekly VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Thursday.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.