May 19, 2017
Massey doctors first in the world to use internal radiation implant to treat pancreatic cancer
Share this story
Doctors at VCU Massey Cancer Center are the first in the world to successfully implant a bio-absorbable, internal radiation device known as CivaSheet to treat early stage pancreatic cancer.
In March, a team of Massey experts led by Emma Fields, M.D., radiation oncologist; Brian Kaplan, M.D., surgical oncologist; and Dorin Todor, Ph.D., medical physicist, completed the procedure on 70-year-old William Grubbs Jr., of Varina, Virginia, and have reported no complications after six weeks.
Grubbs returned for a follow-up appointment with Kaplan more than one month after the seven-hour surgery, and said he felt no pain related to the implantation.
”If I wasn’t told the CivaSheet was there, I wouldn’t know it was inside me,” Grubbs said.
Pancreatic cancer is really the perfect malignancy for the use of this device because the cancer is in a very difficult location, the risk of residual cancer cells following surgery is very high and the disease is very aggressive.
Manufactured by CivaTech Oncology, and supported by the National Cancer Institute, the CivaSheet is a flat, flexible membrane placed in a patient during surgery. It contains a radioactive isotope and provides localized, unidirectional radiation therapy to a targeted area while shielding healthy tissue in the opposite direction.
Internal radiation therapy, also known as brachytherapy, is a form of treatment where higher doses of radioactive material are concentrated at a short distance to kill cancerous cells. It is currently used as a treatment for several cancers throughout the body, however it has not been used for pancreatic cancer until now.
Grubbs was on vacation in Florida this January when he began to feel discomfort that he initially believed to be kidney stones. As the pain continued to worsen, he flew back to Varina and underwent multiple CT scans and an MRI before he was diagnosed with pancreatic cancer.
He was referred to Kaplan, a surgical oncologist. Grubbs said he “never regretted a minute” of his patient experience. With few treatment alternatives on the table, Grubbs placed his trust in his doctor, and elected to move forward with the recommendation of the CivaSheet.
“There is no brachytherapy for pancreatic cancer; there never has been. And there has been no other bio-absorbable, implantable radiation treatment than the CivaSheet,” said Fields, who placed the CivaSheet in Grubbs after Kaplan resected the tumor. “Pancreatic cancer is really the perfect malignancy for the use of this device because the cancer is in a very difficult location, the risk of residual cancer cells following surgery is very high and the disease is very aggressive.”

In 2016, an estimated 53,000 people were diagnosed with pancreatic cancer in the U.S. Almost four out of every five diagnoses are expected to result in death, according to statistics from the National Cancer Institute.
In light of the dismal prognosis and survival rates, recent research performed at Massey supports a shift in the protocol for treating early stage pancreatic cancer. While the standard has been surgery followed by chemotherapy with or without radiation therapy, patients are now recommended to receive a combination of chemotherapy and radiation therapy in the neoadjuvant (pre-operative) setting in order to shrink the tumor prior to surgery. This new approach offers patients another treatment option and an opportunity for a more effective surgery.
The implementation of CivaSheet occurs during the patient’s surgical resection to remove cancerous tissue. In the operating room, after the surgical oncologist has performed the resection, the radiation oncologist will customize and size the CivaSheet to fit the shape of the removed tissue and then place the CivaSheet in the patient’s surgical cavity.
Following surgery, the radioactive isotope Palladium-103 (Pd-103) will organically release radiation from the CivaSheet, directed toward the resected cavity in an effort to minimize cancer cell recurrence.
Because of the radiation shields on the opposite side of the device, the intestines are essentially blocked and protected from the radiation.
The CivaSheet has rows of blue dots embedded by the manufacturer with Pd-103 on the active side to target cancer cells and gold foil on the inactive side, which serves to obstruct all but one-tenth of the radiation from traveling through the body in order to protect sensitive and healthy surrounding tissue.
“The beauty of the CivaSheet is that you can place it face down on the section of removed tissue where the intestines will lay,” Fields said. “Because of the radiation shields on the opposite side of the device, the intestines are essentially blocked and protected from the radiation. With external beam radiation, it’s more difficult to pinpoint the tumor’s location and so it’s harder to protect the intestines to this degree.”
The pancreas is located directly in front of the aorta and several other large blood vessels that branch off to vital organs. It is situated below the liver and behind the stomach. A portion of the small intestine, which is extremely sensitive to radiation, wraps around the head of the organ.
With a half-life of just under three weeks, the Pd-103 will naturally decay between 50 and 70 days, and the sheet itself will be absorbed into the tissue.
Pd-103 is a favorable isotope used for internal radiation therapy because of its low energy and short half-life properties, while still being able to deliver a higher cumulative dosage than other isotopes.

Fields championed the CivaSheet, which was approved by the U.S. Food & Drug Administration in 2014. She said that it should act as a safer procedure for pancreatic cancer patients while minimizing side effects and improving local control of the tumor.
“It’s a win-win. The CivaSheet also doesn’t alter how long a patient waits for surgery or complicate the surgeon’s responsibilities during the procedure,” Fields said.
Although a feasibility study testing the CivaSheet’s safety and efficacy on pancreatic cancer is still awaiting approval, Fields said the device is currently available as an experimental option for all Massey patients.
Once the study is opened in the next few months, there will be a phase 1 clinical trial to analyze vascular toxicity (evidence of harm to the patient’s blood vessels) after two months, and a phase 2 trial to review the rate of cancer growth after one year.
Fields said the goal of the trials is to observe effective local control of cancer growth and prove that the rates of cancer recurrence are lower after the use of the CivaSheet than alternative methods such as external beam radiation therapy. Grubbs’ treatment ahead of the study protocol was helpful in evaluating dosage and toxicities.
Grubbs has since begun physical rehabilitation, and is able to complete simple exercises and short walks to rebuild the muscle he lost following the surgery.
The CivaSheet is just one of many cutting-edge treatment options for pancreatic cancer patients offered through Massey’s recently opened Pancreas and Biliary Neoplasm Program, the first of its kind to the Richmond area to use a multidisciplinary, patient-centered approach to reduce treatment delays and improve outcomes.
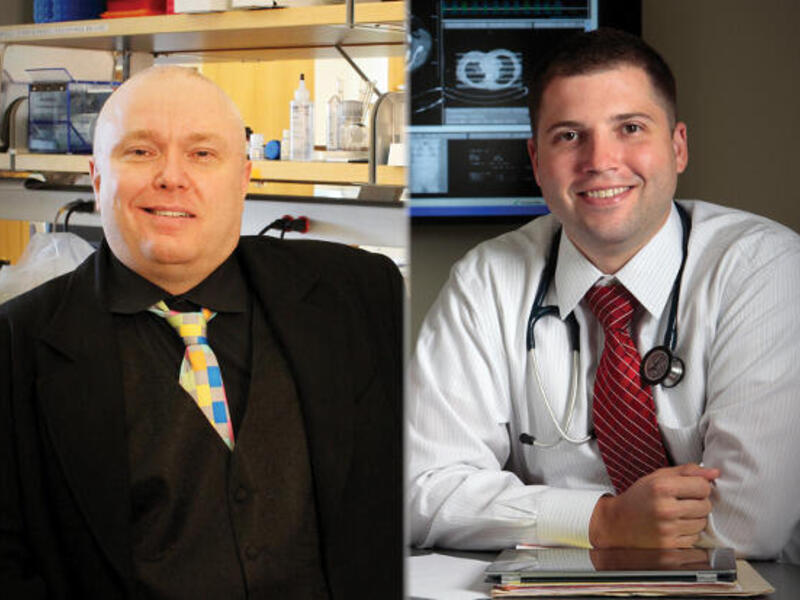
Fields is a member of the Developmental Therapeutics research program at Massey and an assistant professor of radiation oncology at the VCU School of Medicine; Kaplan is the director of the Pancreas and Biliary Neoplasm Program at Massey and a professor of surgery at the VCU School of Medicine; and Todor is the director of the Brachytherapy Program at Massey and an associate professor at the VCU School of Medicine.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.