Jan. 25, 2021
Perfecting the ‘new normal’ in health care
Share this story
As the pandemic brings potentially lasting change to every corner of society, Virginia Commonwealth University researchers are working to capture data around one of the most ubiquitous changes to emerge from the health care world.
Telehealth — where doctors and patients are distant from one another, connected through digital means — can mean anything from a brief phone call to an urgent video conference. Many health care systems went from doing very little of it to integrating it into almost all aspects of care during the pandemic.
VCU Health team members sought to triage potential virus cases remotely. Doctors helped patients with other health issues avoid overwhelming health care facilities. And licensed psychologists across the country found that their therapy sessions quickly jumped from 7% to 85% online.
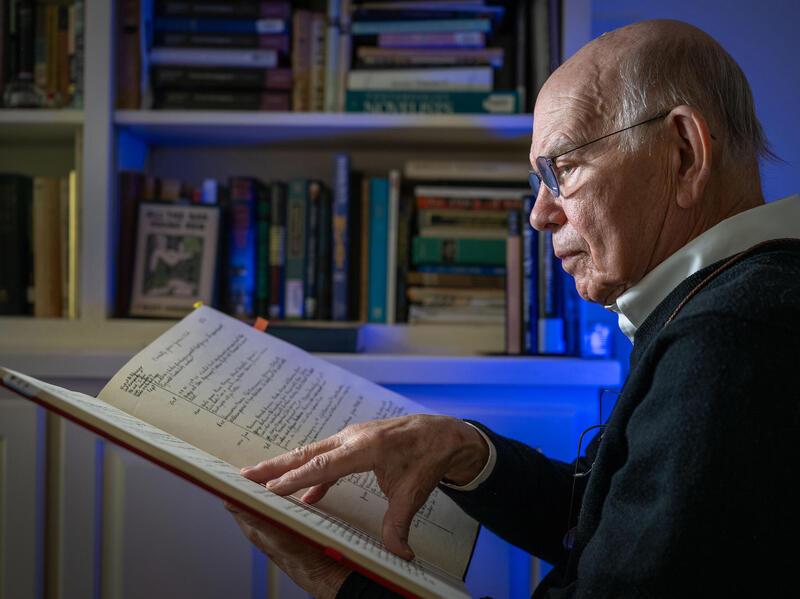
“Telehealth is here to stay,” said Peter Buckley, M.D., dean of the VCU School of Medicine. “But there are gaps in knowledge and questions about it that can and should be studied so that health care providers have guidance and best practices to follow.”
Two researchers will soon answer some of those questions with the help of awards from VCU’s COVID-19 Rapid Research Funding Opportunity. The fund, led by the VCU Office of the Vice President for Research and Innovation with support from the C. Kenneth and Dianne Wright Center for Clinical and Translational Research, awarded nearly $350,000 in funding last spring to 31 VCU research projects that seek to address the impact of the coronavirus.
“We’re seeing a tragic number of excess deaths during the pandemic, partly due to people delaying medical care,” Buckley said. “Telehealth can be a lifeline for patients and doctors — to bridge that gap in care. These researchers will help us understand whether it works, how it works and how we can improve it.”
Reducing stress and social isolation through health coaching
“We’ve gone digital,” and “Online orders only,” said many businesses in the wake of lockdown protocols. When COVID-19 drove people away from public spaces and in-person activities, the internet became an essential utility.
However, that only works if everyone has access to quality internet service.
“Due to the digital divide, in many cases online solutions to connectivity had the opposite effect,” said Faika Zanjani, Ph.D. “It isolated the most vulnerable populations even further.”
The associate professor in the Department of Gerontology in the College of Health Professions designed a project that offers telephone-based health coaching to low-income seniors during the pandemic.
“We all need support,” Zanjani said. “Why not personal health support from the convenience, privacy and social distancing safety of our homes, where we are spending most of our time anyway?”
The seniors reside in subsidized community apartment buildings and are mostly racial and ethnic minorities that the virus has disproportionately affected. Already more vulnerable to the virus itself, the lack of access to internet exacerbates social isolation, food insecurity, the availability of basic needs and undermanaged health.
According to the U.S. Census Bureau, 14% of homes in Richmond do not have a personal computer, and 27% of homes do not have broadband internet access. Low-income elders are most likely to fall into these groups.
Community computer labs in apartment complexes, libraries and other community access centers have closed or may not offer an appropriately confidential space for a telehealth visit.
But the good old-fashioned telephone, Zanjani said, is the most commonly available form of connecting technology. And it’s important, when working with at-risk populations, to use the tools that people have available.
“Health care needs to be inclusive — to ensure everyone has access to the support they need,” Zanjani said.
The findings from her study will support and promote no-contact telephonic health coaching as a means to reduce health risk, stress and social isolation. Zanjani hopes health coaching over the phone will be a useful tool in the emergency preparedness toolbox, a toolbox that multiple VCU researchers have worked to expand in the past year.
“Even with the vaccine, COVID-19 is unlikely to ever be eradicated,” Zanjani said. “And the frequency and intensity of pandemics is expected to continue to increase in the coming century. We need to be prepared to support our more vulnerable populations.”
Telehealth is here to stay. But there are gaps in knowledge and questions about it that can and should be studied so that healthcare providers have guidance and best practices to follow.
Psychological support for young patients and their families
Fear, anxiety, stress, irritability — many people felt these emotions last year.
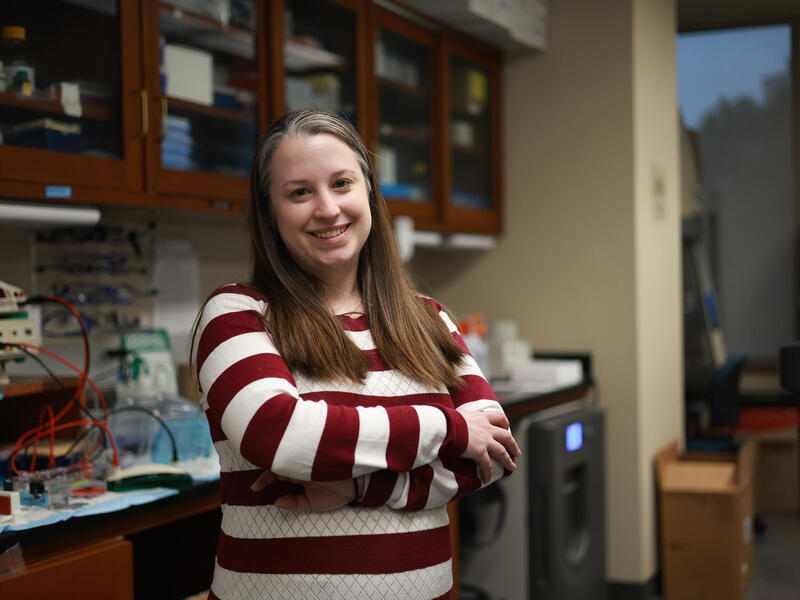
“The pandemic has been physically and psychologically challenging for many people,” said Jennifer Rohan, Ph.D., assistant professor of pediatrics at the VCU School of Medicine. “Especially for young people, adolescents and young adults already struggling with their health.”
Psychological support can help.
Rohan, who is also the director of psychosocial clinical care and research for the Division of Hematology and Oncology at Children’s Hospital of Richmond at VCU, designed a study to offer that support remotely to children who have chronic illnesses such as cancer and blood diseases — and their siblings and caregivers.
Regular, sustained psychological support is crucial to the success of the intervention, and digital platforms like video conferencing can reduce barriers to access, such as unreliable transportation and scheduling. Many patients prefer the flexibility, comfort and privacy of their own homes when talking to a psychologist.
“Patients and families often report difficulties with attending on-site psychological treatment due to having multiple commitments,” Rohan said. “And that limits the clinical effectiveness of psychological interventions.”
The pandemic has heightened the challenge of on-site psychology visits, especially for those with chronic illnesses. Patients, who are often immunocompromised, and their families may avoid medical visits deemed noncritical.
Past research has shown that patients’ attendance improves with telehealth options. Cancellations and no-shows are significantly reduced. And psychologists have found that telehealth services are just as effective, if not more effective, as in-office treatment.
But there’s a gap in research on telehealth with pediatric and adult chronic illness populations. Rohan hopes her project will help determine what specific psychological treatments can be delivered to larger numbers of patients with the greatest positive impact on health outcomes.
Rohan reports that the project is going well.
“Overall, patients and families are coping as well as could be expected during a life full of uncertainties,” she said. “Patients and families have found strategies to maintain their quality of life, including socially distanced peer socialization activities, more time spent in nature, enhanced quality time with family, and more opportunities for virtual connections.”
Telehealth, Rohan said, is about possibilities — ones that go beyond the pandemic. Tailored, preventative interventions that take patients’ needs and challenges into consideration will ultimately improve their health.
Read more about VCU Health and Children’s Hospital of Richmond at VCU’s telehealth services.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.