
July 14, 2020
Virginia doctors recommend a ‘reinvention’ of primary care
Share this story
Primary care doctors were not prepared for COVID-19 and have to reinvent how they practice, say physicians in a paper published Monday in the Annals of Family Medicine.
Alex Krist, M.D., a professor in the Department of Family Medicine and Population Health at the Virginia Commonwealth University School of Medicine, and his co-authors write that primary care practices have a crucial role to play during a pandemic — namely, keeping people out of the hospital.
He said that when COVID-19 hit, primary care providers struggled with a lack of testing and supplies, a lack of unified operations, and financial systems not designed to proactively help communities. Many practices shut their doors and furloughed staff.
“But 75% of Americans have primary care physicians, and 54% of all doctors’ visits are made to primary care physicians," Krist said in an interview. “If you shut your doors, patients are abandoned. They go to overwhelmed emergency rooms, or they avoid the health care system and get sick.”
On the other hand, primary care practices can’t operate as usual during a pandemic. Inviting vulnerable patients into shared waiting rooms endangers patients and staff.
“There’s no road map for how primary care should respond to a pandemic, and the paper outlines the beginnings of one,” said Krist, who wrote the paper with primary care colleagues from Oregon and Northern Virginia.
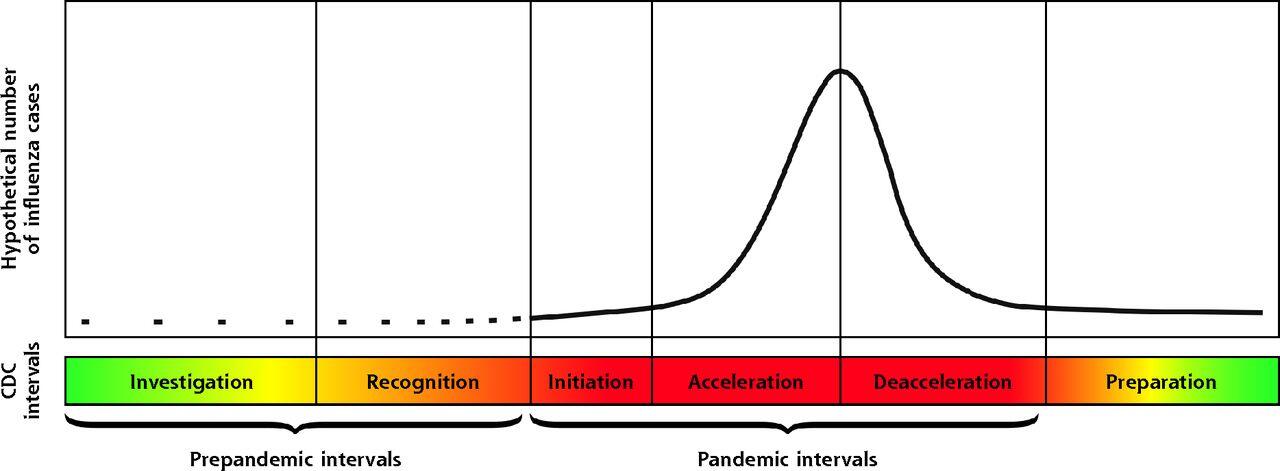
Using a model established by the Centers for Disease Control and Prevention to address outbreaks of flu, “Redesigning Primary Care to Address the COVID-19 Pandemic in the Midst of the Pandemic” recommends several actions for primary care providers at each stage of the outbreak.
Recommendations include early and widespread testing done in the primary care setting and a virtual-first approach to triaging patient care to determine who needs to be seen in person. As hospitals become busy and care for more patients, primary care physicians need to be ready to provide “home hospital care” through virtual monitoring and home visits for sick patients who want to avoid the hospital or cannot go because it’s at capacity. And as a pandemic begins to subside, primary care practices should transition to rehabilitation and support for survivors, tend to the secondary health impacts such as declining mental health and worsening social needs, and address pent-up demand for other health care.
“VCU Health is committed to expanding access to primary care and family medicine programs in a way that integrates with and complements its range of services,” said Peter Buckley, M.D., interim CEO of VCU Health System and interim senior vice president of VCU Health Sciences. “This paper is a great start to an important conversation about the role primary care can play in a pandemic.”
Krist said the paper developed in response to the transformations he’s seen at practices over the past four months. While much media attention has focused on hospitals and intensive care units, primary care clinicians were working hard on the front lines to protect their patients.
“The pandemic was a crisis for primary care,” said Krist, who is also the co-director for community engagement at the C. Kenneth and Dianne Wright Center for Clinical and Translational Research. “Physicians needed to redesign their practices overnight.”
COVID-19 brought three groundbreaking changes to rules around medical care in March. Technology requirements for telehealth were relaxed. Cross-state treatments were allowed. And pay structures were updated to accommodate virtual care.
Primary care practices, though, weren’t prepared for these changes, Krist said. And if the changes stick around, which he hopes they will, physicians need to adapt, especially as COVID-19 infection rates are increasing again.
The paper isn’t just for other doctors, he added. Policymakers, insurers and communities need to continue to support primary care as the first line of defense during a pandemic.
“Primary care is the backbone of our health care delivery system,” Krist said. “And it’s a place where people need to be able to go to have questions answered and needs taken care of, especially during a pandemic.”
Co-authors of the paper are Jennifer E. DeVoe, M.D., of Oregon Health & Science University; Anthony Cheng, M.D., of Oregon Health & Science University; Thomas Ehrlich, M.D., of Fairfax Family Practice; and Samuel Jones, M.D., of Inova Health System in Fairfax, Virginia.
Jones and Ehrlich are faculty at VCU’s Fairfax Family Medicine Residency program, which trains physicians in the evolving clinical world of primary care.
In March, Krist was appointed chair of the U.S. Preventive Services Task Force, a volunteer panel of national health care experts that provides guidance on which preventive services, including checkups and tests, Americans need to stay healthy. Krist is also a co-author on a paper about social determinants of health — economic and social factors that influence a person's health — that was published in the Annals of Internal Medicine on Tuesday by several U.S. Preventive Services Task Force members.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.







