March 27, 2018
Direct-to-consumer cancer testing could be beneficial, Massey expert says, but it’s not a substitute
Share this story
The biotechnology company 23andMe was recently given the green light by the Food and Drug Administration to make direct-to-consumer genetic testing for cancer risk available to the public. The test seeks to identify three specific pathogenic variants in BRCA1 and BRCA2 genes, which are distinctly linked to breast and ovarian cancer in women, and breast cancer in men. After receiving a mailed kit, users can set up an online account with 23andMe and provide a saliva sample that is mailed back to the company and tested.
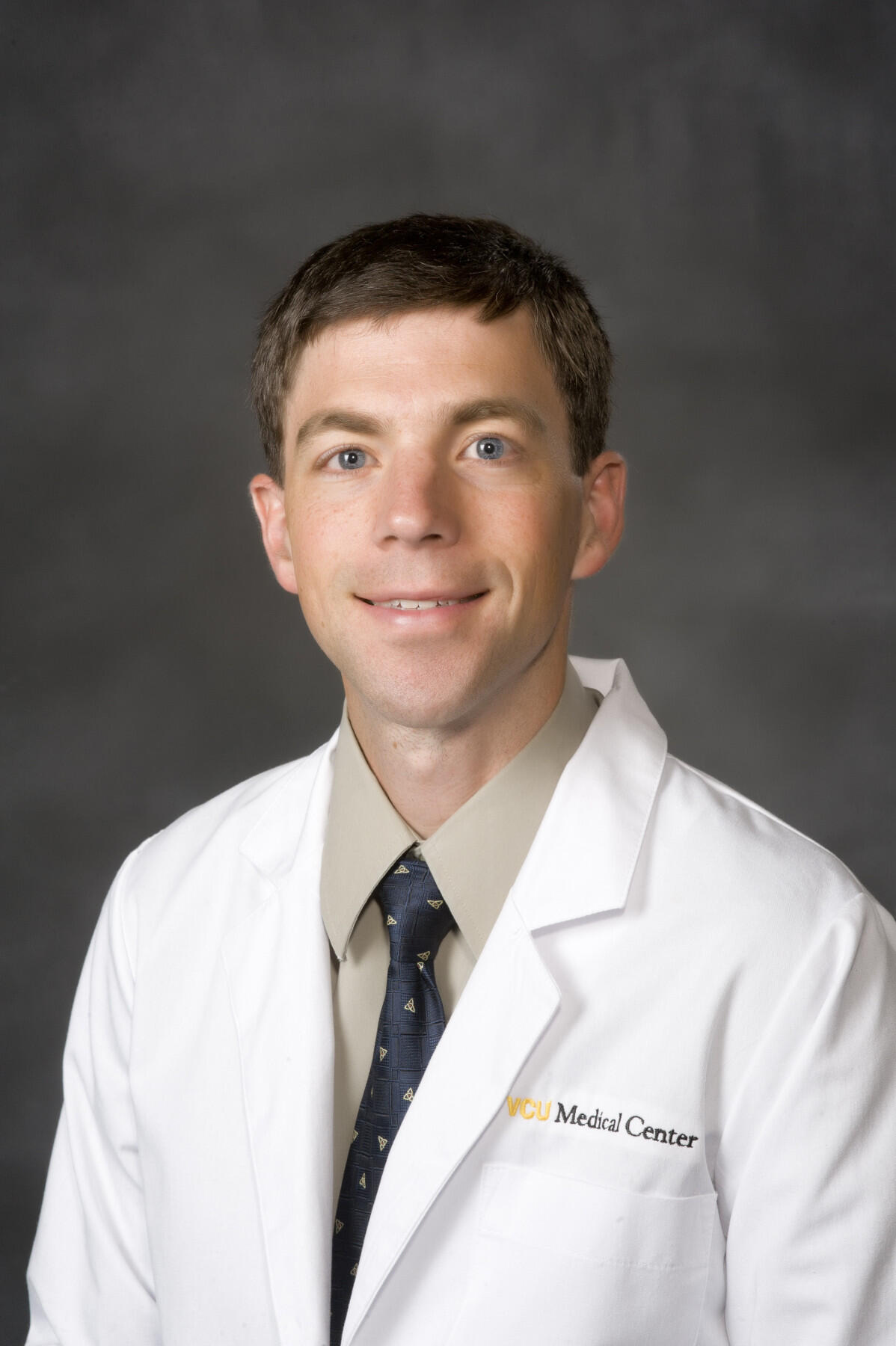
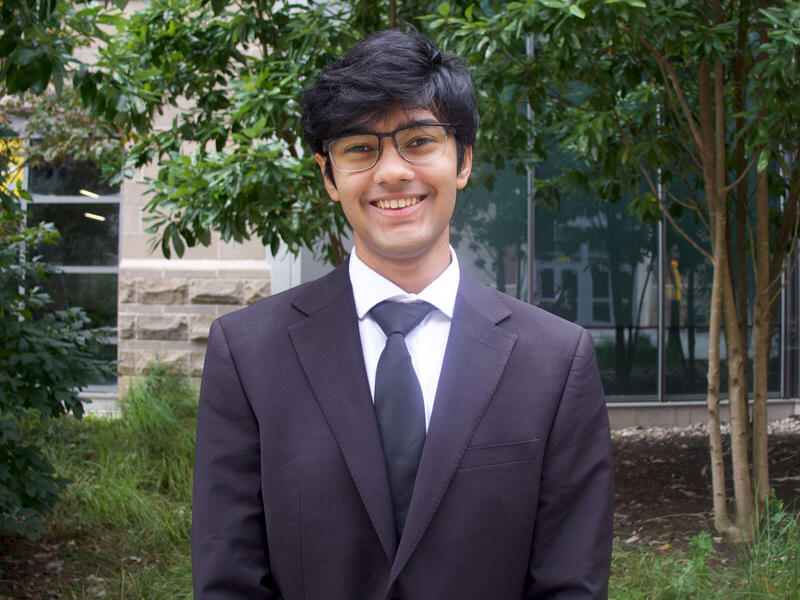
Having this type of testing available to consumers has drawn both acclaim and objection. The FDA stopped similar testing by 23andMe in 2013, because the company had not provided evidence that the test did not jeopardize consumers’ health. John Quillin, Ph.D., a genetic counselor at the Virginia Commonwealth University Massey Cancer Center and an assistant professor in the Department of Human and Molecular Genetics in the VCU School of Medicine, said direct-to-consumer testing has its benefits but it should not dissuade people from implementing the more traditional consultation by a medical professional to address potential hereditary cancer risk.
In response to the FDA’s decision to approve the testing, Quillin offers his medical perspective about the technique and best practices for patients who are genetically susceptible to cancer.
What are the general precautions and concerns that accompany the FDA's approval of direct-to-consumer BRCA testing?
I have heard, and understand, concerns about potential misinterpretation of results or psychological concerns when hearing unexpected or unwelcomed news. Negative results could provide false reassurance since most breast cancer is not associated with BRCA1 and BRCA2, and most people with BRCA mutations do not have ones that would be detected by the 23andMe test. On the other hand, most women with hereditary breast cancer have not accessed genetic testing. Because of limited family structures and inheritance through men in the family, many women with hereditary breast cancer might not know they are at risk. Broad-based, accessible, affordable, direct-to-consumer testing may help increase access and awareness. However, being retested in a clinical setting under the direction of a medical expert is also recommended.
How is this technology different from others that seek to lower cancer incidences and provide early detection?
What is different is the reporting to consumers of high-risk genetic health information, along with a plethora of other information, without the guidance of a health professional. Genetic testing, especially testing as limited as that offered by 23andMe, is unlikely to lower the incidence of cancer by itself, but it could provide lifesaving information if it leads to appropriate high-risk screening or lifestyle changes for people who test positive. It will be important for people who do not test positive to recognize that healthy lifestyles and screening are still important.
What are the most prevalent limitations in this type of testing?
The biggest limitation I see is that it only looks for three mutations that are more common among persons with Ashkenazi Jewish ancestry. Thus, this testing will not likely be useful for most women, even if they have hereditary breast cancer. There may also be some concerns about the accuracy of test results. I reached out to someone at 23andMe who noted that while the FDA affirmed the validity of their test results, 23andMe does not run additional confirmatory testing of positive test results, which typically happens in a clinical diagnostic laboratory. Also, because they are a direct-to-consumer company, they do not have the quality controls for sample collection that would occur in a clinical setting. Also, 23andMe provides contact information for genetic counselors to help with test interpretation, but just providing this contact information does not guarantee access to health care support.
Without this type of testing, how are genetic mutations discovered?
Typically, BRCA1 and BRCA2 testing occurs following pre-test genetic counseling to identify what, if any, genes should be tested and what laboratory techniques are most important. These decisions are made based on personal and family histories of cancer, and what type of information patients want, like their level of risk or medical management plans. While BRCA1 and BRCA2 are the most commonly found genes associated with hereditary cancer, they are not the only ones, so additional testing may be necessary. Once the specific test(s) are selected, patients undergo a process of informed consent. The American Society of Clinical Oncology has recommended this consent process include discussion about several factors such as personal medical implications, family implications, and potential for insurance or employment discrimination.
For how long has VCU Massey Cancer Center offered genetic counseling and what are its general benefits?
Genetic counseling aims to address the medical, familial and psychosocial concerns related to having hereditary risk for cancer.
We have had an established hereditary cancer genetic counseling clinic since 1999. Genetic counseling aims to address the medical, familial and psychosocial concerns related to having hereditary risk for cancer. This information could be helpful across the cancer control spectrum — from primary prevention to making treatment decisions. It is important to note, though, that genetic testing will not be helpful for everyone. It is more likely to be helpful if someone is diagnosed with cancer at a younger than typical age, has had more than one primary cancer, or has had several relatives on the same side of the family with the same type of cancer.
In general, what health precautions should people who are predisposed to cancer take to safeguard their health?
An overall healthy lifestyle is helpful for everyone, including those with hereditary cancer risk. The American Cancer Society’s recommendations include no smoking, eating a minimum of 2 1/2 cups of fruits and vegetables daily, minimizing alcohol, and exercising with at least 75 minutes of vigorous activity or 150 minutes of moderate exercise per week. Screening to detect cancer is often helpful, and people with hereditary cancer may benefit from earlier screening or screening using a different modality, like breast MRI tests for women with hereditary breast cancer risk. Sometimes risk-reducing surgeries or medications can be helpful, depending on the specific hereditary cancer condition.
Subscribe for free to the VCU News email newsletter at http://newsletter.news.vcu.edu/ and receive a selection of stories, videos, photos, news clips and event listings in your inbox every Monday and Thursday during the academic year and every Thursday during the summer.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.