June 2, 2014
Expected California safety-net financial shortfall a gauge for U.S.
Share this story
By 2019 under the Affordable Care Act, California’s safety-net hospitals will experience a shortfall of more than $1 billion annually, according to a study published in the June issue of Health Affairs. The researchers warn that states not expanding Medicaid will fare much worse.
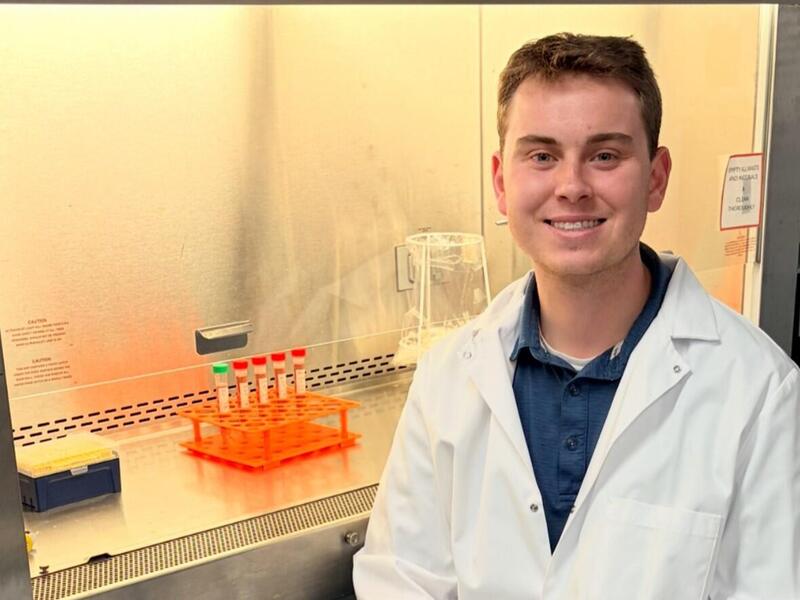
Katherine Neuhausen, M.D., now a faculty member at Virginia Commonwealth University, led the study’s University of California Los Angeles research team as a Robert Wood Johnson Foundation Clinical Scholar.
“The Affordable Care Act will reduce the number of uninsured people and expand access to health care,” said the study. “However, the DSH (disproportionate-share hospital) reductions included in the act, combined with ongoing inflation in the cost of health care, will create funding gaps that must be filled to ensure the financial stability of safety-net hospitals.”
Neuhausen and the research team studied 14 county hospitals in California and six University of California hospitals. The 20 institutions examined received 98.5 percent of the state’s DSH allocation in 2010.
They then estimated total DSH costs for 2019 and found that, while the ACA reduced costs during that time compared to a scenario in which the health care reform law had not been implemented, safety-net hospitals in California could still face $1.381–$1.537 billion in residual uncompensated care costs and Medicaid shortfalls in 2019 under the ACA.
“We found that the rise in total DSH costs at California public hospitals was primarily due to medical cost inflation,” Neuhausen said. “The safety net faces the same challenge of escalating costs that is pervasive across our country’s entire health care system. Public and private hospitals will need to deliver higher value care at lower costs to ensure their financial stability and the country’s fiscal health.”
The researchers offer several strategies that safety-net hospital leaders and state policymakers could consider to close their DSH funding gaps.
One strategy is for state and local leaders to provide additional county and state subsidies to support struggling safety-net hospitals. The study points out that Congress has already delayed the national DSH payment reductions twice, and that another strategy could be to roll back the DSH cuts if hospitals are in jeopardy.
“Our analysis offers lessons for other states,” Neuhausen said. “Safety-net hospitals in states that do not expand Medicaid can expect to fare much worse because they will not receive new Medicaid revenues, and safety-net hospitals in states that do not target DSH payments well could be in jeopardy. If safety-net hospitals are in jeopardy, it threatens the many vital services that these hospitals provide to their communities.”
To read the full Health Affairs article, visit http://content.healthaffairs.org/content/33/6/988.abstract.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.