March 6, 2020
Health expert on limiting coronavirus risk: ‘Get sleep, stay hydrated, wash your hands’
Share this story
Editor's note: This article contains information that may be out of date. Visit VCU Health's COVID-19 page for the latest information regarding the coronavirus outbreak.
COVID-19 — the fast-moving outbreak informally known as coronavirus — continues to spread, increasingly affecting the United States, prompting companies and governments to curtail travel, and throwing global markets into flux. Hospitals and medical centers globally are preparing for its arrival.
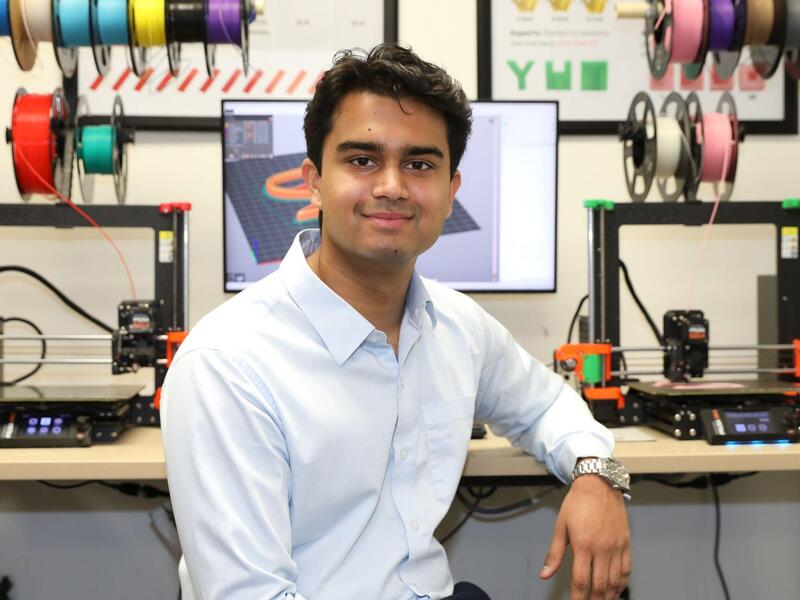
Gonzalo Bearman, M.D., an infectious disease specialist, professor of medicine and director of the VCU Medical Center Infection Prevention Program, spoke with VCU Health News about the virus, what people can do to stay healthy and what they should do if they think they are getting sick.
VCU Health is staying abreast of the situation, Bearman said.
“We are preparing to the fullest extent possible for the arrival of cases to Central Virginia and to our health care system,” he said. “We have policies and protocols in place, but people need to understand that the situation is fluid.”
What are some things that people can do right now to stay healthy and limit the risk of getting COVID-19?
I think the common sense things are to try to be as healthy as possible. Get enough sleep. Stay hydrated. If you smoke, quit smoking. If you drink a lot of alcohol, quit drinking or drink in moderation. Get an influenza vaccine. I realize that doesn't prevent against COVID-19. However, influenza continues to be the clear and present infectious disease danger to Virginia and the United States. So if you can prevent yourself from getting an infection such as influenza, that’ll prevent other infectious disease complications, most likely.
Wash your hands frequently. Learn how to wash your hands, look at our Facebook Live video, or look to the Centers for Disease Control and Prevention for instructional videos on washing your hands. If you have a cough, practice cough and respiratory hygiene or etiquette. Cover your cough, use a tissue, throw it out. And if you’re sick or unwell, please don't go to work and potentially expose others.

Do people who are well really need to wear a mask?
A properly fitted mask will work to reduce the risk of infection or transmission, particularly for health care workers who are wearing them when caring for sick patients. That’s because the health care workers can be very close to the patient.
The benefit of the mask in the community setting — walking on the sidewalk, going for a stroll in the park, going to a concert, or even a flight — is probably much less, even potentially minimal. It's probably having more of a psychological impact than an actual physical transmission-based impact.
Should I still go to the hospital, even if I think I don't have COVID-19 but maybe another illness or disease?
Our hospital is a safe place for care, and we’re here to help you and treat all people. We have protocols and processes in place to keep you safe from health care associated infections, not only things such as COVID-19 but also other more common infections. We’re here to protect you from that while giving you high-quality care.
If you think you have COVID-19, the first step is to call your primary health care provider for guidance on appropriate testing and care.
How and when should you get tested for COVID-19?
It’s important to emphasize that as of March 5, the test isn’t available at the local health care centers or every hospital. It’s still centralized through the state lab, so we have to use it judiciously.
The patient’s symptoms, potential exposure history or travel history, or admission to the hospital with a severe respiratory condition not explained by an alternative or different diagnosis — along with expert assessment or clinical assessment and consultation with our health department colleagues — will ultimately lead to the decision as to whether we test for the new coronavirus. It’s not as simple as walking into your primary care doctor and saying, “I’d like to have my cholesterol checked.” There’s much more nuance, and it’s a combination of the appropriate signs, symptoms and exposure.
What happens if you do recommend that someone get tested?
For [that to happen] the patient has to meet the appropriate clinical criteria, some of the epidemiology criteria, and the doctors assessing the patient have to be convinced that this is a reasonable test to run. Then we work in close collaboration with the health department to coordinate the testing with the state lab. And that patient is given a person-under-investigation number with the health department for the coronavirus test.
There are really two scenarios here depending on how sick the patient is: If the patient is not sick enough to require hospitalization, then the patient is triaged or sent home with oversight by the health department for home quarantine or home isolation until the test is confirmed or ruled out. The other scenario is the patient is sick enough to be admitted to the hospital. If that’s the case, then we use the appropriate protocols in place to make sure health care workers are safe and patients are placed in the appropriate environment. A single room with no roommate, for example, with negative pressure. That means that the air is going into the room and not coming out of the room.
But not everyone who tests positive ends up in the intensive care unit, right?
Correct. That's an important point. To our understanding right now, about 80% of all cases are not serious or not severe, and they don't require hospitalization. Twenty percent are severe enough to require hospitalization. Of that 20%, the minority require intensive care unit level care.
What does home isolation mean?
In general, home quarantine or home isolation is someone staying at home, and in this situation for COVID-19 or the novel coronavirus, for about 14 days. The idea is that by staying at home, monitoring symptoms, they are not exposing others to a potential infectious disease threat. Doing home quarantine has to be done thoughtfully and is typically done in collaboration with the local and state health authorities.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.