Aug. 11, 2016
Medical students travel to Ecuador to help with emergent care
Share this story
When dialing 911 in the United States, callers might easily assume a dispatcher can relay their needs to the appropriate responder, whether it is firefighters or the paramedics. But in Ecuador, it is not always that simple.
From June 27 to July 19 members of the VCU Health International Trauma System Development Program traveled to Cuenca, Ecuador to help enhance the country’s coordination between firefighters, ambulances, 911 call centers and hospitals. The work was part of a series of projects to determine why there is a breakdown in Ecuador’s pre-hospital communication, which starts when a person seeking emergency help contacts authorities and ends when they arrive at a hospital.
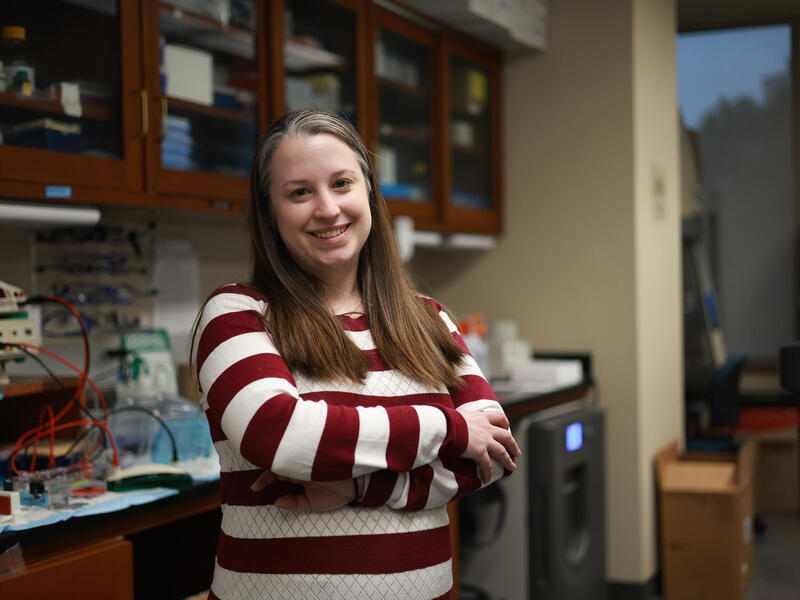
Mark Hopkins, a second-year student in the Virginia Commonwealth University School of Medicine, was one of three medical students who traveled to Ecuador with School of Medicine faculty. Though public health care is free in Ecuador, high patient volume and a lack of resources and proper education dilute the quality of that care, he said.
“Since we were kids, we've known there is one number to call [for medical help] and we know we can trust whoever shows up on our doorstep to be trained and qualified,” Hopkins said. “We have jobs solely dedicated in the hospital to making sure the right information comes through. In Ecuador, they are trying to replicate that system. That’s where we want to help.”
Collecting the data
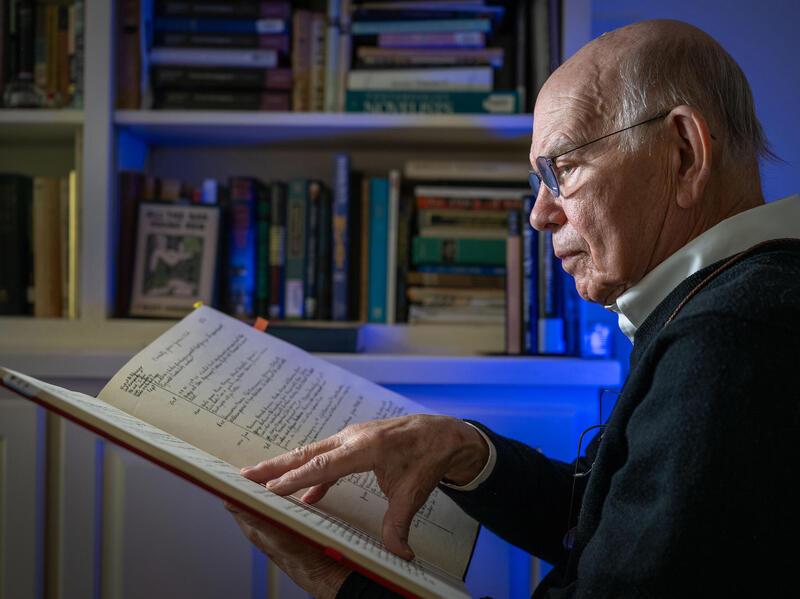
The Ecuador program was developed by Michel Aboutanous, M.D., medical director of VCU Health’s trauma program. VCU Health participants have worked with colleagues at the University of Azuay in Cuenca and the Ecuadorian Ministry of Health since the 1990s. Some of Ecuador’s top health experts — including Juan Carlos Salamea, M.D., a trauma surgeon, and Hernan Sacoto, M.D., dean of the School of Medicine at the University of Azuay — are longtime partners of the program.
Students and faculty this summer researched Ecuador’s ambulance system and taught communication training courses to 350 pre-hospital employees.
As part of their research, the students collected data from emergency medical service personnel and emergency room doctors, listened to patient reports given by personnel and used a developed checklist to see if critical points regarding patient care were passed on correctly.
Their findings resembled a game of telephone, Hopkins said.
“We found that less and less communication was passed on as it went down the chain,” he said. “The immediate information, such as age, gender, and chief complaint was usually given, but other information later on, such as respiratory rates, medications and treatment was usually missed and perhaps viewed as of lesser importance by certain responders.”
Providing trauma care expertise
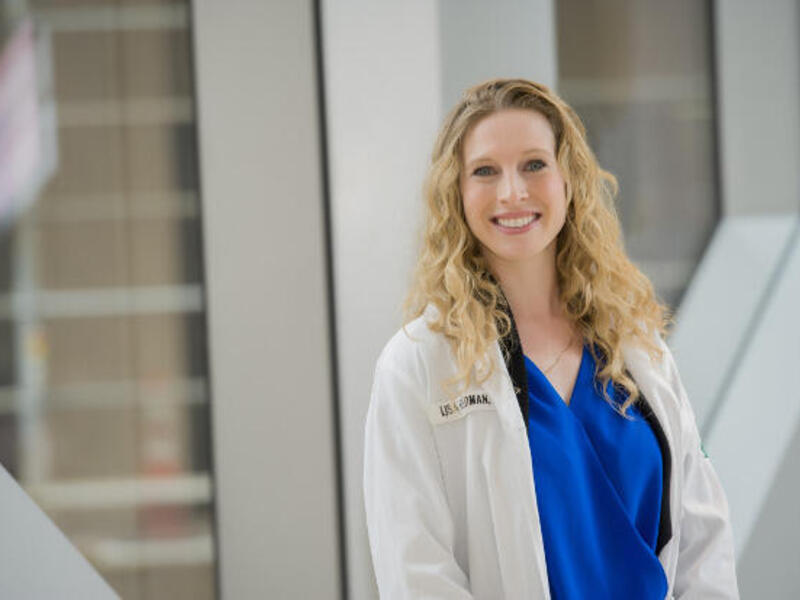
Reasons for these lapses ranged from poorly trained ambulance workers to hospitals being unable to treat patients emergently due to a lack of beds or staff. Sudha Jayaraman, M.D., is an assistant professor and faculty advisor for the International Trauma System Development Program. As the largest trauma center in Virginia, VCU Health is primed to offer its experience in trauma and emergency systems development to health care workers globally, she said.

“We aim to bring our regional experience in trauma and emergency care, and our expertise in global trauma care, to partnerships in various parts of the world, especially since access to emergency care is still a major problem throughout the world,” Jayaraman said.
VCU Medical Center is one of the top trauma centers in the country in terms of trauma volume. The emergency department treats more than 98,000 patients annually, including more than 4,000 trauma patients. VCU Medical Center is the only Level I trauma center in Central Virginia nationally verified by the American College of Surgeons, the highest level of trauma center verification in the United States. The trauma center works closely with the Virginia State Office of Emergency Medical Services and the Richmond Ambulance Authority to support statewide emergency medical services.
“We have a lot of experience here on a major national problem, and we are using that experience to improve care for others around the world,” Jayaraman said.
Hands-on approach
Ecuadorian medical students, with whom the VCU Health group worked, are continuing to teach communication training classes alongside Alberto Martinez, M.D., a physician in Ecuador who facilitates the program’s research. There also are plans to expand the classes to the outer regions of Ecuador. Other next steps include printed information cards being given to Ecuadorian emergency medical service providers, as a reminder of what data to include in the patient report given to hospital staff when a patient arrives.
Many of Ecuador's poorest residents do not receive medical treatment because they live in remote locations. Health care is provided through either private or public institutions. The latter receives less funding on a per patient basis. And, because trauma is the No. 1 cause of death in Americans below the age of 45, global trauma care is especially important.
VCU is glad to have a hands-on approach to helping.
“VCU offers manpower [in Ecuador] in terms of students, experience and consultation on trauma and emergency systems development based on the expertise that we have here,” Jayaraman said.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.