Sept. 22, 2014
New non-invasive technique could revolutionize the imaging of metastatic cancer
Share this story
Bioluminescence, nanoparticles, gene manipulation – these sound like the ideas of a science fiction writer, but, in fact, they are components of an exciting new approach to imaging local and metastatic tumors. In preclinical animal models of metastatic prostate cancer, scientists at Virginia Commonwealth University Massey Cancer Center, VCU Institute of Molecular Medicine and Johns Hopkins Medical Institutions have provided proof-of-principle of a new molecular imaging approach that could revolutionize doctors’ ability to see tumors that have metastasized to other sites in the body, including the bones.
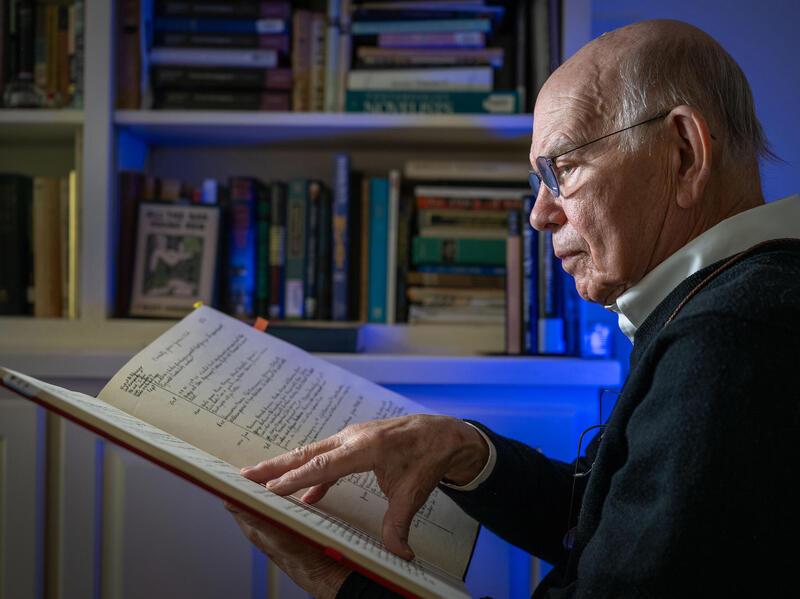
Recently published in the OnlineFirst edition of Cancer Research, a journal of the American Association for Cancer Research,this multiple institution study is the first to develop in vivo (in animal models) a systemically administered, non-invasive, molecular-genetic technique to image bone metastases resulting from prostate cancer. The new method relies on the detection of a gene known as AEG-1, which was originally discovered by the study's co-lead investigator Paul B. Fisher, Ph.D., and has been shown to be expressed in the majority of cancers but not in normal, healthy cells. In preclinical studies, the researchers were able to image bone metastases with greater accuracy than any clinically approved imaging method.
“Currently, we do not have a sensitive and specific non-invasive technique to detect bone metastases, so we are very encouraged by the results of this study” said Fisher, Thelma Newmeyer Corman Endowed Chair in Cancer Research and co-leader of the Cancer Molecular Genetics research program at VCU Massey Cancer Center, chairman of the Department of Human and Molecular Genetics at the VCU School of Medicine and director of the VCU Institute of Molecular Medicine. “Additionally, because AEG-1 is expressed in the majority of cancers, this research could potentially lead to earlier detection and treatment of metastases originating from a variety of cancer types.”
Imaging the expression of a gene in real time is not an easy task. To do it, the scientists used a promoter called AEG-Prom. A promoter is a set of chemical instructions coded in DNA that initiates activity in a gene. The team combined AEG-Prom with imaging agents consisting of a gene that produces firefly luciferase, the bioluminescent substance that makes fireflies glow, and a gene called HSV1tk, which initiates a chemical reaction when specific radioactive compounds are administered. The team then inserted the combination into tiny nanoparticles that are injected intravenously. When exposed to specific proteins that activate the AEG-Prom, including the c-MYC protein that is elevated in many cancer cells, the AEG-Prom initiates activity in the imaging agent, and the location of cancer cells expressing the imaging agent are made visible using sensitive imaging devices.
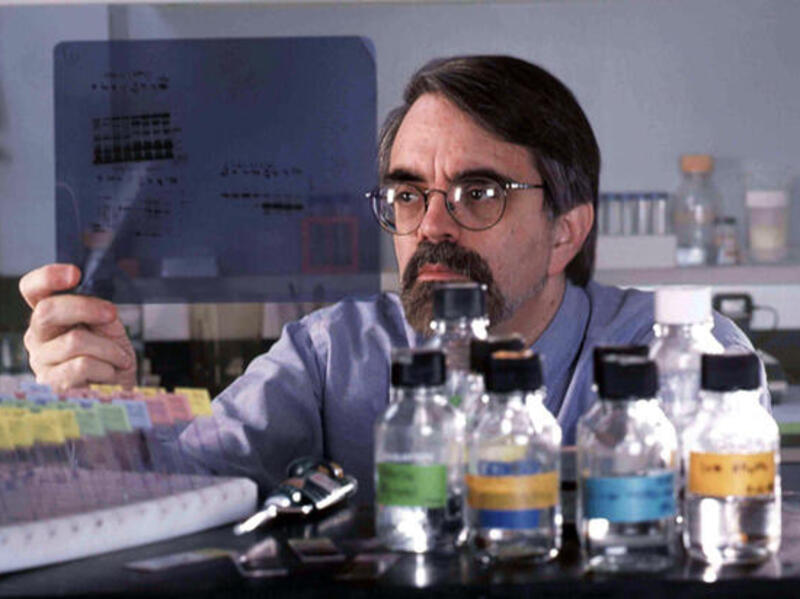
"The imaging agents and nanoparticle used in this study have already been tested in unrelated clinical trials. Moving this concept into the clinic to image metastasis in patients is the next logical step in the evolution of this research," said co-lead author Martin G. Pomper, M.D., Ph.D., William R. Brody Professor of Radiology at Johns Hopkins Medical Institutions. "My colleagues and I are working toward this goal, and we look forward to opening a study to deploy this technology as soon as possible."
Fisher and Pomper are pioneering the use of cancer-specific and cancer-selective gene promoters to image cancer. Previous studies in melanoma and breast cancer leveraged another gene originally discovered by Fisher called progression elevated gene-3 (PEG-3) using a promoter known as PEG-Prom. In addition to imaging, this approach could also be used to deliver therapeutic agents, such as targeted therapies, directly to local and distant tumors sites and allow physicians to monitor drug delivery in real time. Separate studies are currently underway to examine the therapeutic potential of this strategy.
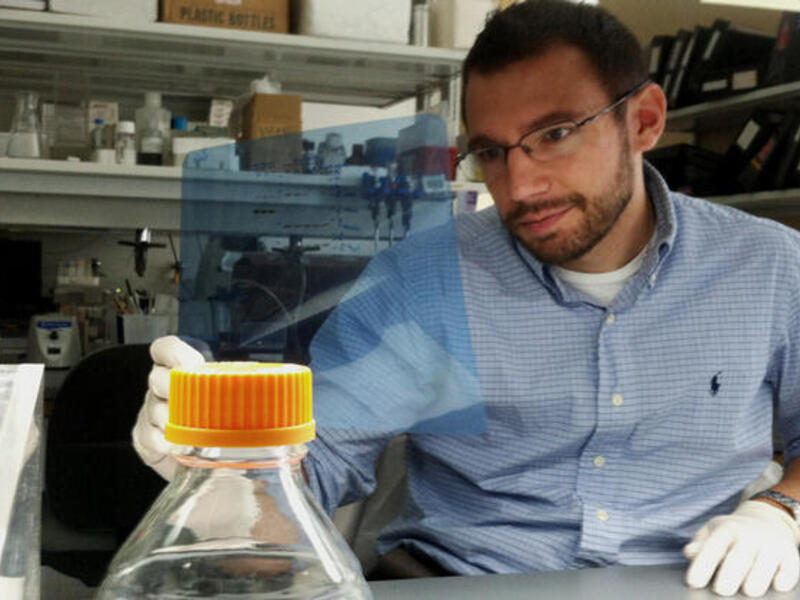
Fisher and Pomper collaborated on this research with Siddik Sarkar, Ph.D., postdoctoral research scientist in the Department of Human and Molecular Genetics at the VCU School of Medicine, as well as Akrita Bhatnagar, Ph.D., Yuchuan Wang, Ph.D., Ronnie C. Mease, Ph.D., Matthew Gabrielson, M.D., Polina Sysa, M.D., lL Minn, Ph.D., Gilbert Green, Brian Simmons, Ph.D., and Kathleen Gabrielson, D.V.M., Ph.D., all from Johns Hopkins Medical Institutions.
This study was supported by National Cancer Institute grant CA151838, the Prostate Cancer Foundation, the Patrick C. Walsh Foundation, the National Foundation for Cancer Research and, in part, by VCU Massey Cancer Center’s NIH-NCI Cancer Center Support Grant P30 CA016059.
The full manuscript of this study is available online at: http://cancerres.aacrjournals.org/content/early/2014/08/21/0008-5472.CAN-14-0018.full.pdf
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.