July 23, 2014
New research findings may lead to better treatment plans for HIV patients coinfected with hepatitis C
Share this story
Using a combination antiretroviral therapy to treat HIV patients coinfected with the hepatitis C virus (HCV) not only effectively treats HIV, but also results in reduced HCV replication, according to a multi-center study published this week in Science Translational Medicine.
The findings advance what is known about the biological effects of patients coinfected with HCV and HIV and may ultimately help physicians improve treatment plans for HIV patients coinfected with hepatitis C. In the United States, coinfection affects approximately 200,000 to 300,000 people; worldwide estimates are between 4 to 8 million people.
Coinfection of HIV/HCV is associated with a higher rate of HCV replication and increased liver injury. Previously, there were concerns in treating coinfected patients with HIV antiretroviral therapy due to possible liver injury.
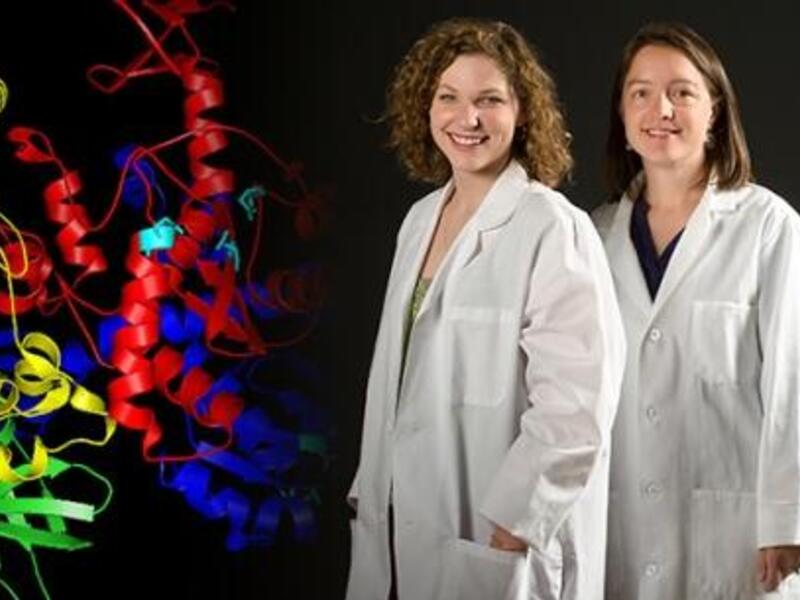
The study was led by researchers at the University of Cincinnati College of Medicine in collaboration with several other medical institutions, including Virginia Commonwealth University.
In the study, researchers closely examined 17 patients coinfected with HIV and hepatitis C who received already approved HIV antiretroviral drug therapies. In order to detect minor changes in the virus and immune response, patients underwent frequent evaluation and provided blood samples during a two-year span.
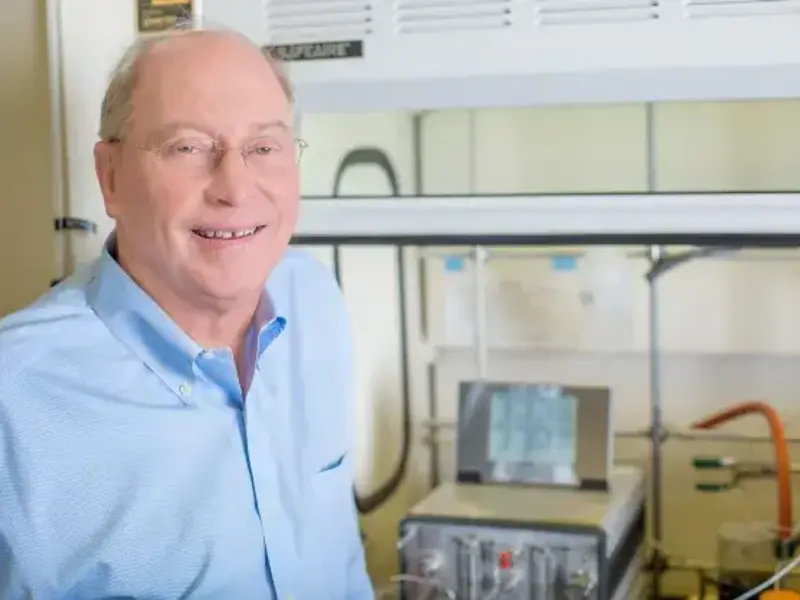
During the first 16 weeks, the team observed an initial increase in a marker of liver injury known as serum ALT, hepatitis C or both. However, according to lead author Kenneth Sherman, M.D., Ph.D., Gould Professor of Medicine and director of the University of Cincinnati Division of Digestive Diseases in the College of Medicine, during a period of 18 months, researchers found that viral loads for HCV returned to what was expected in a monoinfected patient suffering from HCV without HIV. Initial liver injury actually resulted from effective HIV treatment and not from toxicity.
In a statement released by the University of Cincinnati, Sherman said, “Initial response to HIV treatment results in a transient increase in HCV viral replication and evidence of liver injury. However, over time HIV suppression leads to reduced HCV replication.”
“Because we used to think that increases in liver enzymes and HCV were harmful to coinfected patients starting HIV treatment, many providers caring for those with HIV got nervous which led to early discontinuation of lifesaving HIV treatment,” said the principal investigator for the VCU portion of the study, Richard Sterling, M.D., professor of medicine, chief of hepatology and medical director of HIV-liver disease at VCU.
“This carefully done study tells us that these transient changes are not harmful and provide reassuring data to both patients and providers,” Sterling said.
According to Sterling, future studies are needed to help tease out the mechanisms of why liver enzymes and HCV increase during this early period of starting HIV therapy.
“The data from this study tells us that treating the HIV first is safe in those coinfected. This is important as newer treatments for HCV are soon available that are not only much better tolerated, but also require a much shorter course of therapy, with higher response rates exceeding 90 percent and similar to those without HIV,” he said.
The study was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences. Portions of this work were performed under the auspices of the U.S. Department of Energy.
The paper is titled: “Modulation of HCV replication after combination antiretroviral therapy in HCV/HIV coinfected patients.”
Subscribe for free to the weekly VCU News email newsletter at http://newsletter.news.vcu.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.