March 21, 2018
New VCU report shows death rates are rising in Virginia’s white population
Share this story
Societal issues are driving an increase in death rates among Virginia’s white population, according to a new report from Virginia Commonwealth University’s Center on Society and Health. Stress-related conditions—including unintentional drug overdoses, suicides, alcoholic liver disease and alcohol poisonings—are killing white Virginians ages 25-54 at increasing rates.
Death rates have generally decreased in the United States and other industrialized countries in the past century. The VCU study sought to examine the factors responsible for recent mortality trends in the white population, hoping to address the public health crisis in that demographic and examine health trends that could affect other groups. The report helps underscore the importance of addressing the root causes of poor health, including social, economic and environmental conditions, and of adopting policy solutions that can ensure opportunities for optimal health among Virginians of all backgrounds.
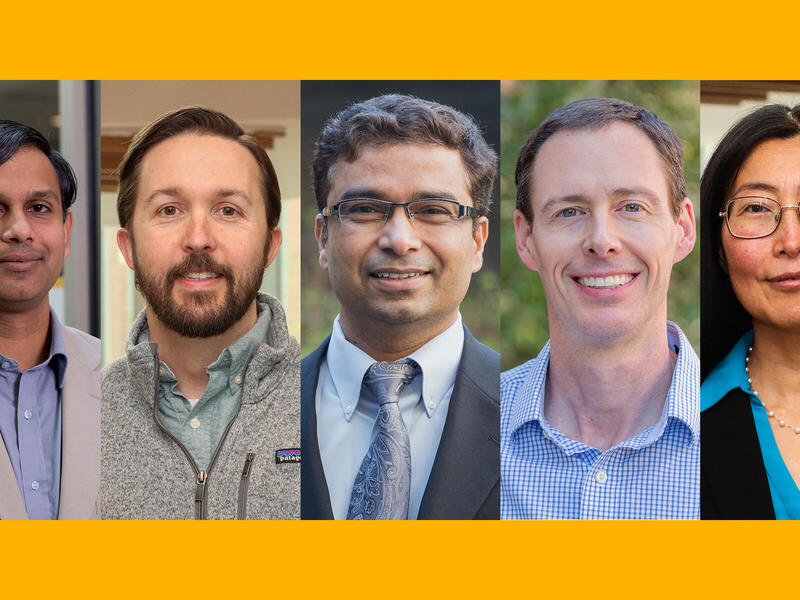
“The alarming rise in death rates from drug overdoses, alcoholism and suicides demands action,” said Center on Society and Health Director Steven Woolf, M.D., who is a professor at VCU School of Medicine. The Center on Society and Health is an academic research center that studies the health implications of social factors – such as education, income, neighborhood and community environmental conditions, and public policy. Previous Center research has found that African-American and Hispanic communities in Richmond, Northern Virginia, and other areas of the state have shorter life expectancies and disproportionate exposure to living conditions that harm health.
“The need for policies to improve living conditions and economic opportunity for Virginia’s most vulnerable populations could not be more urgent,” Woolf said.
The report, which emphasizes that populations of color often experience higher death rates than white populations, theorized why middle-aged white people might be disproportionately impacted by rising mortality rates. “This age group is experiencing life conditions that differ starkly from past expectations and may lack the resilience to endure the cumulative stress that comes with prolonged social and economic hardships,” the authors wrote, noting that during the two decades examined in the report, young and middle-class white people experienced economic and social instability unlike that of their parents and grandparents.

The report that published March 21 reveals that stress-related deaths among white people ages 25 to 54 increased 83 percent between 1995 and 2014. The report also highlights other trends, such as statewide increases in deaths from organ diseases, which are possibly linked to substance abuse and trauma. These include liver cancer, viral hepatitis and some forms of heart disease, among others. The researchers examined eight regions of Virginia, including all 95 counties and 38 independent cities.
Between 1995 and 2014, the increase in the death rate due to stress-related conditions caused nearly 2,300 deaths among white people ages 25 to 54. At a 331 percent increase, the rise in death rates from unintentional drug overdoses was startling, Woolf said, but there also were increases in alcoholic liver disease (37 percent) and suicides (29 percent) among young and middle-aged white people.While the report focused on Virginia, these findings mirror a nationwide trend, which some refer to as “deaths of despair.”
The report authors noted that, while rising death rates among white people warrant investigation, death rates in certain minority populations continue to be persistently and alarmingly higher than their white counterparts. From 2010 to 2014, the death rate among African-Americans in Virginia was still 1.2 times higher than that of the white population.
“This crisis underscores the urgent need for policy action to reduce health inequities for all Virginians,” Woolf said.
The report found that the highest increases in death rates among white people due to stress-related conditions occurred in Southwest, Southside and West Central Virginia, areas that have endured persistently high poverty rates for many years. Across Virginia, those areas with the largest increases in death rates tended to be rural and less diverse, have higher percentages of adults without bachelor’s degrees and higher unemployment rates, and have a shortage of mental health professionals. “This is a crisis of our household economies and our communities,” Woolf said. “It will not be solved simply by changing how painkillers are prescribed.”
However, mortality increases due to stress-related conditions did not solely affect rural localities. Areas of Northern Virginia and Hampton Roads also saw increases from the same causes of death. As the authors expressed in the report: “Hardship exists not only in rural Virginia but, increasingly, in pockets of disadvantage in metropolitan areas. More nuanced explanations for these health trends must also be considered.”
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.