April 8, 2020
What does loss of smell mean during COVID-19?
Share this story
As the novel coronavirus COVID-19 continues to spread, many patients are reporting a loss of sense of smell and sometimes taste as a symptom. As many as 85% to 88% of patients in a study recently accepted to the European Archives of Oto-Rhino-Laryngology reported smell and taste dysfunctions in mild-to-moderate cases of COVID-19.
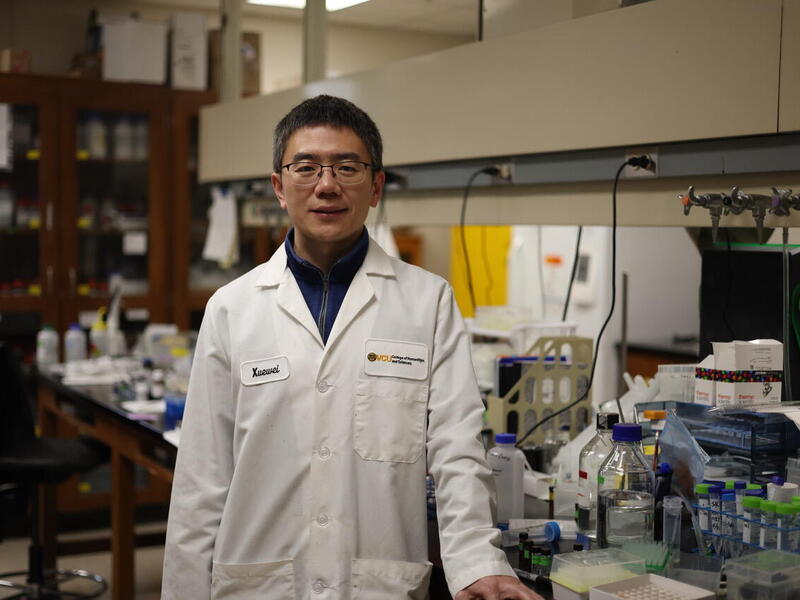
Virginia Commonwealth University experts on anosmia, or loss of sense of smell, say that while the connection needs more study, COVID-19 patients’ reported loss of smell is a trend worth noting. VCU School of Medicine faculty Richard Costanzo, Ph.D., professor emeritus in the Department of Physiology and Biophysics, and Evan Reiter, M.D., professor in the Department of Otolaryngology - Head and Neck Surgery, have decades of experience working with patients who experience anosmia.
Together, they run the Smell and Taste Disorders Center at VCU Health, Costanzo as its research director and Reiter as its medical director. The center is one of few nationwide that consults with patients to evaluate and manage smell and taste disorders. It opened in 1980 so doctors and researchers could work with patients who experienced anosmia from head injuries, but the center now sees patients with smell losses from a variety of causes. Recent years have seen an uptick in the number of cases related to viruses, Costanzo said.
Reiter, Costanzo and VCU co-researchers Professor Daniel Coelho, M.D., and third-year medical student Zachary Kons began conducting a study on smell and taste loss in patients with COVID-19 on April 6.
Reiter and his team encourage those who’ve experienced changes to their sense of smell or taste this year or who have had a COVID-19 diagnosis to access and participate in the survey.
VCU News spoke to Costanzo and Reiter about how to tell the difference between allergies and COVID-19, how long it takes for sense of smell to return in other cases of anosmia, and what to do if you have concerns about a loss of smell.
Is the loss of smell or loss of taste an early sign of COVID-19?
Costanzo: It could be, but it has not been adequately studied scientifically so we don’t know for sure. But there seems to be a link between anosmia and COVID-19, as a large number of cases have been reported. Whether that is an early sign, a predictor, is not known for sure.
There seems to be a link between anosmia and COVID-19, as a large number of cases have been reported.
Reiter: One of the confounding issues here is that you’ve got a significant percentage of patients who have mild disease who may not be aware of even being infected or when they were infected, and then one of their first symptoms or, in some cases, even their only symptom may be a change in their sense of smell. So it’s hard to say if that’s an early symptom, not knowing exactly when they contracted the virus.
Are there other potential causes of loss of smell?
Costanzo: If people think that, “Oh, if you lose your sense of smell, it means you have COVID-19,” there are a lot of people that will notice, if you bring to their attention, that their sense of smell is not that good. Especially in the elderly, it’s a common occurrence as people get older and there are other conditions that can cause a loss of smell. So to call it a predictor of COVID-19 is premature.
Reiter: Yes. Given that there are a lot of people who are presumed positive but are not being tested, there are other respiratory viruses still around, including flu itself. And some of these other viruses, including rhinoviruses — which are commonly implicated in the common cold — other coronaviruses and influenza, also have been implicated in causing a loss of sense of smell.
For people who are having this symptom, when do you think they can expect to start to recover their sense of smell, if at all?
Reiter: On one hand, I’ll say it’s a little bit of uncharted territory because we wouldn’t really know exactly how this particular virus will behave. But with other causes of loss of sense of smell, including with other viruses, it can depend on a number of factors, such as the severity of the loss. The nerves of the sense of smell can regenerate, and with that, the sense of smell can be restored even in people who have a complete loss. But that recovery of nerves is very slow, so that can take up to a year or a year and a half for it to recover. That’s not saying, by any means, that everyone is going to recover, but just that, for those who are going to recover, it may take that length of time. Presumably, with a milder injury, it can be a little bit of a quicker process, but that’s unknown right now.
What complications can arise when the sense of smell is recovering?
Reiter: One potential issue with recovery from a significant loss of sense of smell can be a distortion of smells. All parts of the system may not recover at the same time and to the same degree. Any complex odor isn’t going to just trigger a response in one receptor. It’s going to trigger responses in a number of different kinds of receptors. And your brain integrates all that information together to say, “Well, that’s a rose,” or “that’s chocolate.” In some people, if they have a significant loss, some of the receptors may recover, whereas others may not, or some may recover to different degrees. That can lead to distortions of odors so things that previously were pleasant odors may be unpleasant. And in rare cases we’ve seen, people can have severe food aversions because they get incomplete recovery of their sense of smell, and it causes such distortion that really leads to appetite problems.
If I have recently noticed a sudden loss of my sense of smell, do I definitely have COVID-19?
Reiter: I can’t say you definitely have COVID-19, but given the current prevalence right now, I’d say odds are that yes, it’s going be COVID-19 to some degree. Also, with the risks involved with transmission, we would tell patients to assume it’s COVID-19 until proven otherwise.
Costanzo: If you had told us that you were recently in an accident or fell down and hit your head or you had, for example, changed your medications just a couple of days ago and noticed your sense of smell changed, there are certain things that we would look for that might cause the change in sense of smell that are unrelated to COVID-19.
How can patients tell the difference between loss of smell due to allergies versus COVID-19?
Reiter: Well, there’s no perfect solution, but we are seeing that COVID-19 doesn’t have a very high incidence of nasal issues, such as congestion and runny nose, that sort of thing. Symptoms like congestion, sneezing, runny nose certainly would point more toward allergies.
If I experience loss of smell, what should I do? Should I call my doctor? Self-quarantine? What’s the best next step for me?
Reiter: If there are no other obvious causes such as a head injury, I think self-quarantine is a reasonable step. I think calling your doctor would be reasonable to see if they can test for the virus, or what their thoughts are. Otherwise, just in the name of safety, I think self-quarantining for two weeks would make sense.
The rough number that I keep seeing thrown about is roughly 80% are mild cases. Now that’s not to say all 80% are asymptomatic, but not fitting the bill of the high fevers, respiratory distress and severe aches and pains and needing to seek medical attention and even hospital admission.
Is there anything else that you think is important for people to know about this topic?
Costanzo: I think the underlying theme is that we don’t know enough yet about this virus and that, although there are a lot of reports, it’s important to approach this in a careful way and proceed forward based on facts and data.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.