Feb. 27, 2019
Virginia is well prepared to handle Medicaid expansion, VCU studies find
Share this story
Earlier this year, Virginia became the 33rd state to expand Medicaid, giving nearly 400,000 low-income residents access to affordable health insurance. Two new Virginia Commonwealth University reports examine how prevalent substance use disorders are among Virginia’s uninsured, and how well the state is prepared to take care of those newly eligible Medicaid members with a history of substance use.
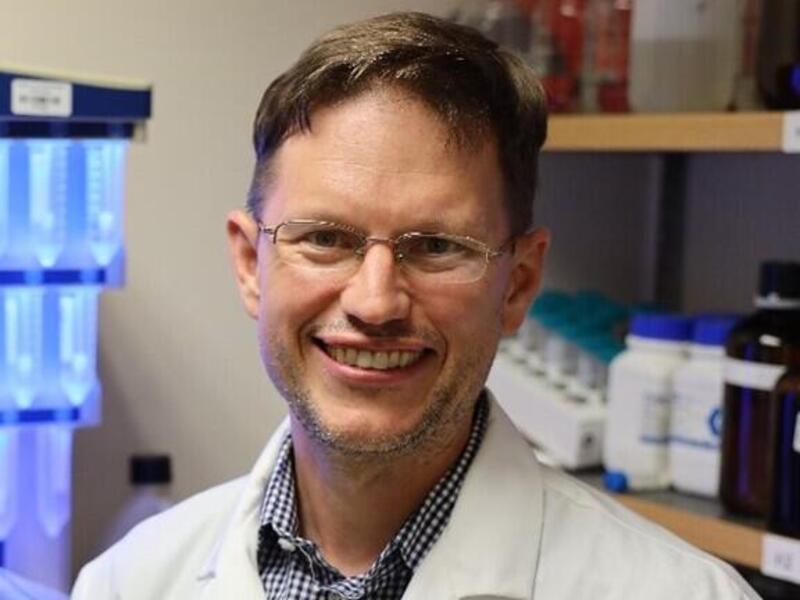
In 2017, the Virginia Department of Medical Assistance Services selected VCU to lead a five-year evaluation of ARTS, a state program designed to enhance Medicaid-sponsored treatment services for substance use disorders to address the rise of opioid-related deaths in Virginia. Peter Cunningham, Ph.D., a professor in VCU School of Medicine’s Department of Health Behavior and Policy, is leading the evaluation along with Andrew Barnes, Ph.D., also from the Department of Health Behavior and Policy.
The ARTS evaluation reports suggest that Virginia is “well prepared,” according to Cunningham, to manage more people in need of addiction treatment services who are newly eligible for Medicaid services.
“Medicaid expansion in other states has not made the addiction crisis worse, but better, according to available data,” Cunningham said. “Virginia has successfully implemented limits on opioid prescribing. Combined with efforts to increase addiction treatment services through the ARTS program, the state is well prepared to handle Medicaid expansion.”
“We found that more than 100,000 uninsured Virginians reported illicit drug or alcohol abuse or dependence in 2016 and 2017,” Cunningham said. “And two-thirds of those with an opioid use disorder did not have health insurance. Medicaid expansion could give as many as 60,000 uninsured Virginians access to treatment services for substance use disorders through ARTS, including 18,000 with an opioid use disorder.”
For its projections, VCU used 2016 and 2017 estimates from the National Survey on Drug Use and Health and applied them to Virginia. The national survey explored the prevalence of substance use disorders among the uninsured, as well as how many uninsured had family incomes below 138 percent of the federal poverty level, the income threshold for Medicaid expansion eligibility in January 2019.
Many of the treatment options will be available outside the hospital setting, aiming to reduce the number of admissions related to substance use. “When you don’t have health coverage and treatment options in your community, you often end up ill enough to require hospitalization. In 2016, one in three hospital admissions among uninsured residents were related to substance use,” Cunningham said.
More than 230,000 Virginia adults are now covered and receiving medical services under the new Medicaid expansion eligibility rules, said Jennifer S. Lee, M.D., director of DMAS.
“This historic accomplishment means that thousands of individuals struggling with addiction now have access to high-quality care through the ARTS program for opioid and other substance use disorders,” Lee said. “With more than 440 provider organizations offering lifesaving care to Virginia Medicaid members through ARTS, we are confident that we can have a significant impact on the opioid crisis in our commonwealth.”
Other key findings in the reports:
Demand for substance use treatment services may peak in West-central Virginia.
This region of the state, including cities such as Lynchburg, Roanoke and Salem, will likely see the greatest increase in demand for treatment services.
“This part of the state has a high share of uninsured residents who are likely eligible for Medicaid expansion and a high rate of uninsured hospital admissions related to substance use disorders, which suggests high prevalence among the uninsured,” Cunningham said.
Based on the share of uninsured Virginians with a family income threshold that qualifies them for Medicaid expansion, new demand for treatment services may be highest in Southside (46 percent) and far Southwest Virginia (43 percent).
Opioid prescribing rates dropped significantly when quantity limits and prior authorization took effect in 2016.
The Centers for Disease Control and Prevention has established a link between high opioid prescribing rates and overdose deaths. High average doses and long prescription periods increase the number of opioids supplied per prescription, placing patients at greater risk for opioid use disorder and overdose. Opioid prescribing rates dropped significantly when quantity limits and prior authorization took effect in 2016.
“Addiction treatment starts with prevention, so our evaluation also looked at how prescribing practices in the commonwealth have changed to prepare for Medicaid expansion,” Cunningham said.
In Virginia, the total days supplied of prescription opioids decreased by 66 percent between 2012 and 2018, from 335.5 days to 114.7 days per 100 Medicaid members. The pace of decline has accelerated since 2016 when DMAS implemented prior authorization guidelines and quantity limits for chronic pain prescription opioids for all Medicaid members.
“We have also seen less doctor shopping among Medicaid members for prescription opioids, which likely reflects in part greater use of the state’s Prescription Monitoring Program,” Cunningham said.
The number of members receiving an opioid prescription has also dropped, from more than 83,000 Medicaid members in 2012 to 42,985 members in 2018.
Providers have increased co-prescribing of naloxone, a medication designed to reverse the effects of an overdose.
While fewer members are receiving opioid prescriptions, more of them receive co-prescriptions for naloxone, an “opioid antagonist” used to reverse the effects of opioid overdose. In the first quarter of 2018, more than 1,000 Medicaid members who received opioid prescriptions also received naloxone. In comparison, almost no Medicaid members received a naloxone prescription with their opioid medication in the first quarter of 2016.
Other School of Medicine collaborators for the 2019 ARTS evaluation updates include Yaou Sheng, Huyen Pham, Heather Saunders, Erin Britton, Augustus White and E. Marshall Brooks, Ph.D. Lauryn Saxe Walker, a senior economic adviser at DMAS, contributed to the report while working as graduate research assistant at VCU.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.