May 17, 2023
Fighting fentanyl
Share this story
Researchers and scientists at Virginia Commonwealth University and VCU Health are charging ahead to find the answer to a decades-old opioid crisis that, in Virginia, now claims more lives than automobile accidents and guns combined.
The most potent killer is fentanyl.
Fentanyl kills more adults ages 18 to 49 nationally than car accidents, suicides, guns or falls, according to a recent Washington Post report that drew from 2021 data from the Centers for Disease Control and Prevention.
A dramatic rise in synthetic opioid-related deaths that started during COVID-19 spurred several actions by the federal government, including a $1.5 billion aid package announced last fall that provides, among other things, increasing access to overdose medicines like naloxone for first responders.
That was followed by the announcement in late 2022 of a new website that would be updated every two weeks with nonfatal opioid overdose data, collected at the county level in all 50 states from emergency medical systems’ first responders.
Joining the fight is Yan Zhang, Ph.D., professor of medicinal chemistry at the VCU School of Pharmacy and a member of the VCU Institute for Drug and Alcohol Studies.
In July 2022, Zhang was awarded a $2.8 million grant from the National Institute on Drug Abuse to advance his research into the development of specific opioid receptor antagonists that would reverse the acute and chronic toxicity of fentanyl. This year, he was awarded an additional $4.3 million from NIDA to expand and continue that work for three more years.
His grants underscore VCU’s status as a leading research institution for opioid use disorder. Last year, VCU was awarded $16.5 million in NIDA funding, placing it 18th nationally.

While he has dozens of research grants to his name, these are Zhang’s second and third grants in recent years pertaining to opioid use disorder. He also received an NIH/NIDA grant in 2019, worth just over $2 million, for development of novel mu opioid receptor modulators, with the goal of conducting preclinical studies on several novel lead compounds for opioid use disorder treatment. Mu receptors are among a family of critical proteins in the body that modulate pain, but major side effects from the application of common mu opioid receptor agonists — such as morphine and fentanyl — are abuse and addiction, and even overdose.
“We want to develop a more effective treatment for fentanyl overdoses that tackles the interaction between fentanyl and mu opioid receptors,” Zhang said.
Potent Problem
Fentanyl packs a dangerous punch. It’s 100 times more potent than morphine and at least 30 times more potent than heroin.
It’s often reserved to treat the most severe cases of acute and chronic pain. Like other opioids, fentanyl targets mainly mu opioid receptors, which are found on cells throughout the body. When opioids attach themselves to these receptors, they block the body’s pain receptors in the brain, stimulating its pain management mechanisms. They also send waves of dopamine into the brain, creating feelings of euphoria — the sort of high that leads patients to addiction.
Medical supervision is imperative, as a few milligrams of fentanyl are enough to kill an adult. Research shows that as little as one week’s worth of fentanyl can lead to addiction, especially for those who may be genetically predisposed to it.
Yet for many who use opioids outside of a doctor’s watchful eye, access is as easy as ordering the drugs by mail, and use can lead to a variety of side effects including death.
Opioid misuse can produce a variety of gastrointestinal issues such as nausea and vomiting, along with fatigue. But the most serious side effect is respiratory depression — shallow breathing and an irregular or slow heartbeat — which can lead to death, Zhang said.
He described the opioid crisis as needing a three-pronged solution. In layman’s terms, he said, this means improving lives, changing lives and saving lives.
Improving lives means finding effective, nonaddictive pain management medications that minimize the risk of addiction when individuals are first introduced to opioids, usually as patients in the hospital.
The grants he’s secured support research for the other two stages — changing and saving lives. He explained that changing lives means developing effective medications for those who are already addicted but working through therapy. His 2019 grant supported this research.
His current research focuses on the direst stage of the crisis — the overdose. He’s working to develop a chemical counteragent that will block fentanyl’s ability to attach itself to the mu opioid receptors. Part of the challenge is tackling not only fentanyl’s toxicity, but also polysubstance abuse addiction, where fentanyl is mixed with other opioids.
Overdose deaths involving fentanyl often occur not from fentanyl alone — it’s often added to other street drugs, unbeknownst to users.
“When they are mixed together, the scenarios can be very difficult to tackle as researchers,” Zhang said. “If you make something that responds to fentanyl, it will also have to respond to other substances that the fentanyl is mixed with.”
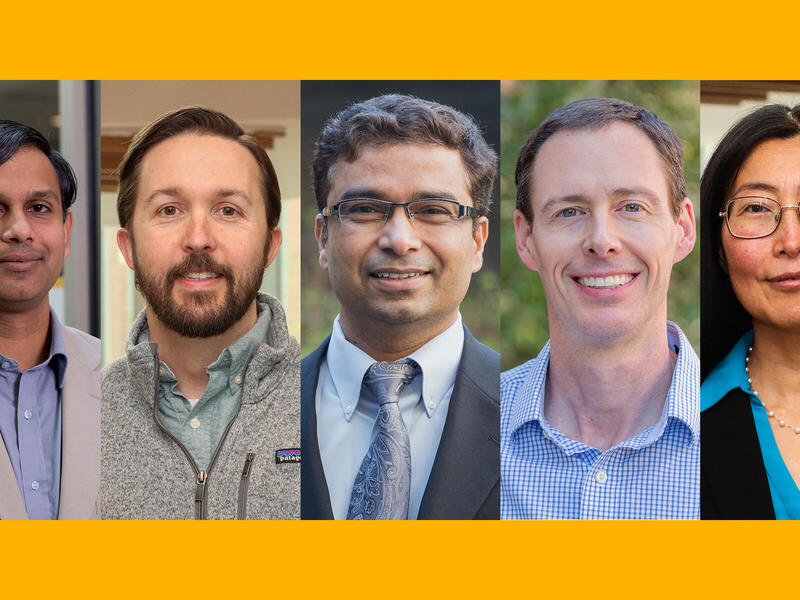
Zhang is working with an expert team at VCU and VCU Health of chemists, biologists and pharmacologists. Within that team is psychiatrist and addiction expert F. Gerard “Gerry” Moeller, M.D., director of VCU’s Wright Center for Clinical and Translational Research and the university’s associate vice president for clinical research. Moeller also leads the VCU Institute for Drug and Alcohol Studies.
Moeller echoed Zhang, in that increasingly today, overdoses often have a common element: the presence of fentanyl.
“Fentanyl is really potent so if you’re not tolerant to opioids, it’s very easy to overdose,” Moeller said. “Fentanyl can be put into other things in really small amounts and have a big effect.
“We’re seeing overdose deaths with cocaine, for example, but it’s not from the cocaine itself,” he added. “It’s the fentanyl being added to the cocaine.”
Naloxone is the go-to medication for overdoses, but it has its limitations, Zhang said.
“Your body metabolizes very quickly so the naloxone will disappear, but the fentanyl lives on in your body, maybe for several hours,” Zhang said, “which means you have to be given multiple doses of naloxone.”
The danger doesn’t go away once an individual survives an overdose. In fact, it’s the opposite. After one overdose, “the odds of you having a repeat overdose and dying are really high,” Moeller said.
Moeller said all these elements — from research capabilities and in-house programming to involvement in statewide initiatives — have positioned VCU as a global leader in combating addiction and specifically, opioid use disorder.
“There’s been a great shift in the history of the overuse of prescription opioids and that’s very positive,” Moeller said. “At VCU, we’re in the next phase, which is how do we treat the significant number of individuals who have opioid use disorder and keep them from becoming a statistic.”
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.