Oct. 10, 2018
A study in the science of play: Does early engagement help premature babies thrive?
Share this story
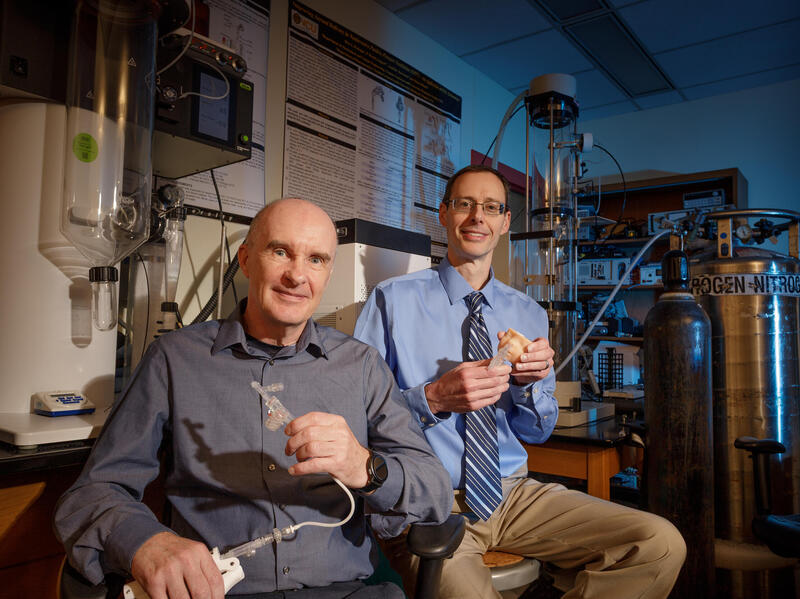
Infants born very preterm, at or before 28 weeks gestation, are at high risk for developmental impairments. Physical therapy and medical specialists from Virginia Commonwealth University are leading a study in collaboration with colleagues from the University of Virginia to determine how early, evidence-based physical therapy intervention can enhance physical, social and cognitive outcomes.

The team of researchers was awarded a $2.84 million grant from the National Institutes of Health to facilitate the multi-site clinical trial, “Efficacy of Motor and Cognitive Intervention for Infants Born Preterm (SPEEDI2).”
The program is based on two smaller studies using Supporting Play, Exploration and Early Developmental Intervention (SPEEDI) developed through a series of studies at Children’s Hospital of Richmond at VCU. Stacey Dusing, Ph.D., a board-certified pediatric physical therapy specialist and associate professor in the Department of Physical Therapy at VCU and the Department of Pediatrics at CHoR, is the principal investigator for the project and the impetus behind the study concept.
“Bringing a new baby home is always a bit daunting, but particularly so following a lengthy stay in the neonatal intensive care unit,” Dusing said. “I did a series of studies that involved going to the homes of babies who were born prematurely and noticed a big gap between parents’ comfort level and the potential of what they could be doing with, and for, their babies. My goal is to determine the best way to help these families support their babies’ development from the very beginning.”
SPEEDI2 uses guided participation to empower parents in reading their infant’s behavioral cues, identifying ideal times for interaction and enriching the learning environment. The study will enroll a total of 90 infants from the NICUs at CHoR and UVA beginning in January. Participants will be randomly assigned to one of three groups — usual care, SPEEDI2 intervention starting in the hospital and lasting for four months, or SPEEDI2 intervention starting at four months post baseline (approximately three months after discharge from the hospital). Both SPEEDI2 groups will receive 10 visits with a physical therapist and 12 weeks of daily play-based intervention by the parent.
The two smaller SPEEDI studies were funded by Children’s Hospital Foundation, the Foundation for Physical Therapy and the College of Health Professions Research Incentive Program. Qualitative feedback from parents was instrumental in securing funding for the larger program. This feedback included feeling a better connection with their baby and confidence in positive engagement techniques.
“Based on this parental feedback on the smaller studies and basic science research, we believe the earlier the intervention the better the outcomes at 12 and 24 months,” Dusing said. “The question of timing hinges around whether new parents need a period to transition home from the NICU, or if earlier intervention during the transition to home will help them immediately establish developmentally supportive routines. In addition to improved motor and cognitive outcomes for baby, we expect that SPEEDI2 will have a significant positive impact on parents’ mental health. Specifically, we will be looking at parental stress level as part of the study.”
The investigative team includes specialists in physical therapy, neonatal medicine, neurology and biostatistics.
In early October, Dusing received a $50,000 Endowment Fund from the VCU C. Kenneth and Dianne Wright Center for Clinical and Translational Research. The fund supports meritorious pilot and feasibility research.
Dusing will apply the fund toward a supplemental research effort called the SPEEDI2 Brain Behavior Study. “The purpose of the project is to evaluate the feasibility and collect pilot data on the efficacy of the SPEEEDI intervention in infants with different types of brain injuries and determine the feasibility of measuring neuroplacitiy changes following early and intensive intervention,” Dusing said.
With the Wright Center support, Dusing will enroll eight-to-10 infants who are also enrolled in the SPEEDI2 study to be evaluated for neuroplastic changes following early and intensive intervention. The research team will use a MRI scanner that is housed at the Children’s Hospital of Richmond at VCU to conduct the additional research.
“Research from the past decade has demonstrated that the brain is adaptable and experience can change the brain’s structure in positive and negative ways,” Dusing said. “With this research, we hope to begin to evaluate if it is feasible to measure early brain plasticity in the first six months of life. If we are able to measure these changes, we can begin to determine if early intensive and targeted physical therapy can elicit positive changes in the brain, which may reduce the rate of long-term disability.”
For more information about SPEEDI2, including inclusion criteria and outcome measures, visitclinicaltrials.gov/ct2/show/NCT03518736. For more information about the Motor Development Lab in the Department of Physical Therapy at VCU visit pt.chp.vcu.edu/research/research-labs/motor-development-lab/.
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.