Aug. 15, 2018
Midlife mortality rates are increasing across U.S. racial-ethnic populations, VCU-led study finds
Share this story
Midlife mortality rates in the United States have increased across racial-ethnic populations for a variety of conditions in recent years, offsetting years of progress in lowering mortality rates, according to a Virginia Commonwealth University-led study. “Warning Signs: Changes in Midlife Death Rates Across Racial and Ethnic Groups in the United States” will publish in The BMJ (formerly the British Medical Journal) on Aug. 18.
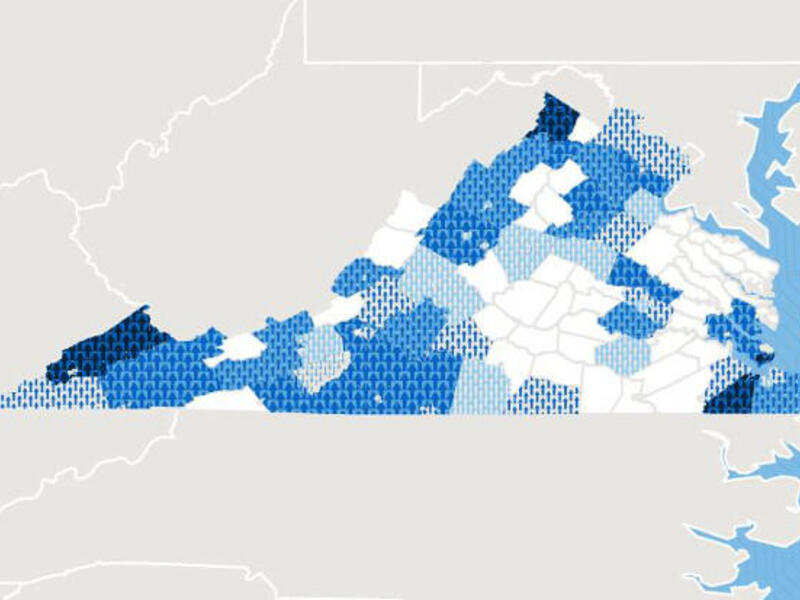
In the report, researchers demonstrate that midlife death rates rose significantly between 1999 and 2016 not only among whites, which previous studies had documented, but also among people of color, including Hispanic and non-Hispanic American Indians and Alaska Natives, African-Americans and Asian and Pacific Islanders. The data for many conditions show a reversal in progress, in which mortality rates that had been decreasing among populations of color reached a nadir and then increased in recent years. In fact, death rates for some conditions are accelerating faster among nonwhite people than among the U.S. white population.
Drug overdoses, alcoholism and suicides were major contributors to the trend, but the new research shows that death rates also increased for dozens of organ diseases such as hypertensive heart disease and liver cancer.

“The opioid epidemic is only the tip of the iceberg,” said lead author Steven Woolf, M.D., director emeritus of the VCU Center on Society and Health. “Death rates are also increasing for diseases involving the heart, lung and other body systems. The trend is too broad to blame on one cause.”
Drawing on data from the Centers for Disease Control and Prevention’s National Center for Health Statistics, the researchers systematically compared U.S. mortality patterns across racial and ethnic groups between 1999 and 2016 among people ages 25-64. They aimed to document responsible causes of death and track each cause’s relative contribution to excess deaths. It was the first study of its kind to examine vital statistics for this time period in such detail. The VCU researchers conducted the study in partnership with colleagues at the University of Pittsburgh Graduate School of Public Health.
U.S. life expectancy has been decreasing since 2014, according to the NCHS. Previous research has attributed the decrease, which follows years of lengthening life expectancy, to rising mortality rates among white people ages 25 to 64. Conventional explanations for the trend have included rises in fatal drug overdoses, alcoholic liver disease and suicides. The trifecta of midlife mortality causes are commonly referred to as “deaths of despair.”
“Our research indicates that the ominous mortality pattern that began for some groups in the 1990s is now unfolding among people of color,” Woolf said. “No racial group has been spared.”
In the report, the researchers warned that the data signal an unfolding public health crisis and implored policymakers to take action.
“That death rates are rising throughout U.S. populations for dozens of conditions signals a systemic cause and warrants prompt action by policymakers to address the factors responsible for declining U.S. health,” Woolf said. “This study reaffirms the pervasiveness of the previously reported systemic causes for the U.S. health disadvantage. We need to examine not only deficiencies in health care and the prevalence of risky behaviors, but also socioeconomic inequalities, unhealthy environmental conditions and detrimental public policies.”
Subscribe to VCU News
Subscribe to VCU News at newsletter.vcu.edu and receive a selection of stories, videos, photos, news clips and event listings in your inbox.